ADHD Brain: What to Know About Symptoms of ADHD — and How to Cope
Struggling to stay focused, meet deadlines, or keep your thoughts from racing? You’re not alone, and these could be signs of Attention Deficit Hyperactivity Disorder (ADHD), a condition that affects both children and adults in unique, often misunderstood ways. Let’s break down the symptoms, science, and everyday strategies that can help you navigate life with more clarity and self-understanding.
What Is ADHD
ADHD, or Attention-Deficit Hyperactivity Disorder, is one of the most common neurodevelopmental disorders, typically beginning in childhood and often continuing into adulthood. It’s not a personality flaw or just “inconsistent behavior.” People with ADHD have brains that process information, regulate attention, and manage impulses differently. And that difference is real, measurable, and supported by decades of scientific research.
You may have heard the term ADD (Attention Deficit Disorder) too. Today, ADD is considered an outdated term. Current understanding of ADHD is that it comes in different “types”, one of which is primarily inattentive (what used to be called ADD). But not all of them.
At the core of ADHD is executive dysfunction — meaning challenges with things like organizing, starting tasks, following through, and self-monitoring. People with ADHD often struggle to focus on boring tasks but may “hyperfocus” on something they find exciting. That’s not a contradiction, it’s part of how the ADHD brain manages attention differently.
Understanding what ADHD really is helps break the stigma. It’s not about being lazy or scattered. It’s a brain-based condition, and it deserves special care.
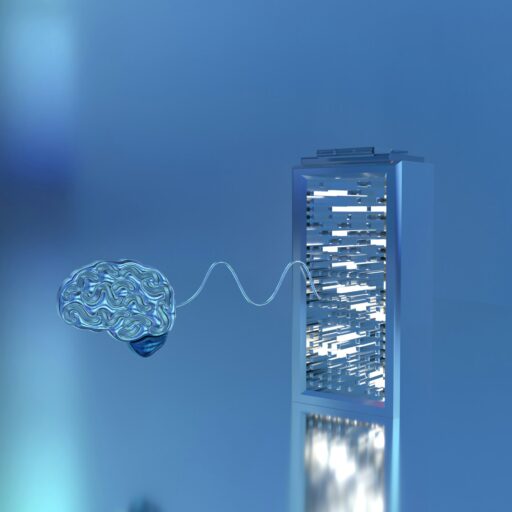
What is ADHD Brain
People with ADHD are neurodivergent, meaning their brains develop and function differently from those who are neurotypical, whose brains develop and work in the typical or expected way. In people with ADHD, brain imaging studies have shown differences in several regions, particularly those linked to executive function, attention control, and the reward system.
One key player here is dopamine — a hormone and neurotransmitter involved in motivation, attention, and pleasure. In “ADHD brains”, dopamine signaling tends to be lower or less efficient. That means everyday tasks that require sustained focus or delayed gratification, like doing taxes or answering emails, can feel physically harder to engage with. It’s not about willpower. It’s chemistry.
There are also differences in how people with ADHD perceive time, regulate emotions, and manage working memory. Some may describe ADHD as “having 100 browser tabs open at once” or “knowing what you need to do, but being unable to start.”
These brain-based differences explain why traditional productivity tips or pep talks often fall short. ADHD isn’t about not trying hard enough, it’s about having a brain that’s wired to work differently, especially in modern environments full of distraction.
Types of ADHD
There are three official subtypes of ADHD, and they can look very different in real life:
- Inattentive type: Often quiet, distracted, disorganized. This is the daydreaming student or the adult who forgets meetings and zones out mid-conversation.
- Hyperactive-Impulsive type: Restless, talks fast, interrupts, acts before thinking. Think blurting out in meetings or trouble sitting still in a movie.
- Combined type: Features of both inattentiveness and hyperactivity/impulsivity.
ADHD also presents differently by gender. Females with ADHD are often diagnosed later than males and tend to have higher rates of depression and anxiety both before and after their ADHD diagnosis. People with the predominantly inattentive type of ADHD usually receive their diagnosis later than those with the hyperactive-impulsive type, and they are also more likely to be diagnosed and treated for mood disorders like depression.
Ultimately, it’s not about fitting into a box. It’s about noticing how your brain works, how it impacts your life, and what tools can help.
What ADHD Feels Like
People with ADHD can experience different symptoms, ranging from mild to severe, depending on its type. Someone with inattentive ADHD may find it hard to concentrate, often losing track of details or forgetting appointments. Meanwhile, a person with hyperactive-impulsive ADHD might feel constantly restless, struggle to stay still, or act without thinking.
For many, it feels like their brain is juggling too many racing thoughts at once, with no clear way to focus or prioritize. Alongside this mental overload, emotional swings can add another layer, ranging from sudden excitement to deep frustration.
Even among adults diagnosed with the same type, challenges can look very different. One person might struggle mainly with procrastination and keeping things organized, while another battles a “mental ping-pong” that jumps rapidly from one thought to another, making it hard to focus during conversations. Though they share the same diagnosis, their day-to-day struggles can feel worlds apart.
Living with ADHD is challenging, but with understanding and tailored strategies, it’s possible to channel its unique energy and build a life that fits your brain’s rhythm.
Main Symptoms of ADHD
Though ADHD shows up differently in adult people, all forms share a common root: challenges with regulating attention, impulses, and behavior over time. Here’s how the symptoms typically show up:
- Inattention – Difficulty staying focused, especially during tasks that require mental effort or lack immediate reward.
- Forgetfulness – Losing track of appointments, objects, or conversations, even when they’re important.
- Disorganization – Trouble managing time, prioritizing, or keeping things in order, at home or at work.
- Poor follow-through – Starting projects with energy but struggling to finish them or maintain momentum.
- Hyperactivity – Feeling restless, needing to move constantly, or talking excessively.
- Impulsivity – Speaking without thinking, interrupting others, or making quick decisions without considering consequences.
- Emotional reactivity – Strong mood swings or frustration over small things, often with slow recovery time.
Understanding the type of ADHD someone has can make a big difference in finding the right strategies to support them. Many people, especially women and adults, go undiagnosed for years because their symptoms don’t match the loud, restless stereotype. But every type is valid and treatable.
How Common Is ADHD
ADHD is one of the most common mental health conditions, especially in children, but it doesn’t always “go away” with age. In fact, about 5–8% of children are diagnosed with ADHD worldwide, one-third of them meet the full diagnostic criteria into their 20s, and around 65% continue to experience impairing symptoms.
Historically, ADHD was viewed as a “boys’ problem,” mostly tied to hyperactivity. But now we know that ADHD often shows up differently in girls and women. That means a lot of people were missed or misdiagnosed growing up. What’s changing is awareness, and many adults are realizing they may have had ADHD all along. The rise in ADHD diagnoses isn’t just a “trend” or overreaction — it reflects growing awareness and improved methods for identifying ADHD.
Still, while TikTok and social media can be helpful by putting words to lived experiences and connecting people with ADHD, they can also create confusion. A 2025 study published in PLOS One journal found that fewer than 50% of claims about ADHD symptoms in popular #ADHD TikTok videos align with clinical standards, highlighting why professional assessment and diagnosis remain essential.
Causes and Risk Factors of ADHD
ADHD isn’t caused by bad parenting, too much screen time, or lack of willpower. It’s a complex condition rooted in brain development and shaped by both genetics and early environmental influences. Here are some of the key risk factors researchers have identified:
- Genetics – Having a close relative, such as a parent or sibling, with ADHD or another mental health condition significantly raises the likelihood of developing ADHD.
- Prenatal substance exposure – Being born to a parent who used recreational drugs, alcohol, or tobacco during pregnancy may affect fetal brain development and increase ADHD risk.
- Premature birth – Being born too early (before 37 weeks) can interfere with early brain development and has been associated with a greater likelihood of ADHD.
- Environmental toxins – Exposure to substances like lead — often found in old paint or plumbing — has been linked to a higher risk of attention and behavioral problems.
While these factors don’t directly cause ADHD, they can increase a child’s vulnerability to developing it — especially when combined with other biological and environmental influences over time. Conditions like chronic stress, family conflict, or a lack of structure may also intensify existing symptoms of ADHD or contribute to delays in recognizing them.
Is It Really ADHD — or Something Else
It’s not uncommon for ADHD to be mistaken for other conditions — and vice versa. Many of the symptoms associated with ADHD, such as inattention, restlessness, forgetfulness, or emotional overwhelm, also show up in situations involving high stress, burnout, or anxiety. That’s why a thorough assessment by a qualified professional is so important.
Here are some conditions that may be confused with ADHD:
- Chronic stress or burnout. Ongoing stress, especially related to work or caregiving, can impair focus, memory, and emotional regulation, closely mimicking ADHD symptoms.
- Generalized anxiety disorder (GAD). Anxiety can cause racing thoughts, distractibility, and irritability. Unlike ADHD, these symptoms are often driven by persistent worry or fear.
- Depression. Low mood, fatigue, slowed thinking, and difficulty concentrating are all common in depressive disorders and can be misread as signs of ADHD.
- Sleep disorders. Poor sleep quality or conditions like insomnia or sleep apnea can lead to attention problems and daytime hyperactivity, especially in children.
- Autism spectrum disorder (ASD). Though it can co-occur with ADHD, autism has its own set of traits, including challenges with social communication and restricted or repetitive behaviors.
- Learning disorders. Difficulties in reading, writing, or math might look like inattention or lack of effort, but stem from specific cognitive challenges rather than ADHD.
- Sensory processing issues. Being overly sensitive or reactive to stimuli can lead to distractibility and emotional dysregulation, sometimes mistaken for ADHD.
- Bipolar disorder. Periods of high energy, impulsivity, and mood shifts in bipolar disorder can resemble ADHD, but the timing and intensity of symptoms differ.
If you’re wondering whether it’s ADHD or something else, timing, context, and consistency matter. ADHD symptoms usually show up in childhood and persist across different settings — school, home, work, or relationships. In contrast, symptoms triggered by stress or another condition may be more situation-specific or episodic.
Getting an accurate diagnosis means looking at the full picture, not just the symptoms.
What Conditions May Be Linked With ADHD
ADHD often exists alongside other mental health or developmental conditions. While it doesn’t directly cause these issues, children and adults with ADHD are more likely than their peers to experience overlapping challenges. Recognizing these co-occurring conditions is essential for providing the right support — and avoiding missed or mistaken diagnoses.
Common conditions that may occur with ADHD include:
- Oppositional defiant disorder (ODD) – A pattern of persistent defiance, irritability, and resistance to authority figures, often leading to frequent conflicts at home or school.
- Conduct disorder – More severe behavioral issues involving aggression, lying, stealing, or violating the rights of others.
- Disruptive mood dysregulation disorder (DMDD) – Intense mood swings and chronic irritability, with difficulty managing frustration or emotional reactions.
- Learning disabilities – Difficulties with reading, writing, math, or language comprehension that can interfere with school performance and self-esteem.
- Substance use disorders – A higher likelihood of misusing alcohol, nicotine, cannabis, or other substances as a way to cope with emotional or attentional struggles.
- Anxiety disorders – Excessive worry, fear, or nervousness that may impact sleep, concentration, and daily activities.
- Obsessive-compulsive disorder (OCD) – Recurring intrusive thoughts and repetitive behaviors that feel impossible to control and often cause significant distress.
- Mood disorders – Depression or bipolar disorder, marked by prolonged sadness, irritability, or episodes of elevated energy and impulsive behavior.
- Autism spectrum disorder (ASD) – A developmental condition affecting communication, social skills, and behavior, sometimes overlapping with ADHD traits.
- Tic disorders – Involuntary movements or vocalizations (such as blinking, throat-clearing, or grunting) that may appear suddenly and vary in intensity.
Because these conditions can mask or mimic ADHD symptoms, a comprehensive evaluation is key. With the right diagnosis and support plan, many of these challenges can be effectively managed alongside ADHD.
Treatments for ADHD
ADHD is treatable, and there are many support options from behavior therapy to medication. CBT (Cognitive Behavioral Therapy) is well known for helping with emotional regulation, managing distractions and creating routine, even for kids. Then, there’s ADHD coaching focused on building practical skills and routines tailored to how your brain works.
Medication like stimulants that increase dopamine and improve focus is a common and effective step. Non-stimulant options also exist, especially for people with anxiety or sensitivity to meds. Sleep hygiene, meditation, different forms of mindfulness — like mindful movement — and structured environments do help a lot. You may consider digital tools like apps and habit trackers designed to help you set and achieve short- and long-time goals.
Remember that treatment for ADHD isn’t about becoming “normal.” It’s about thriving with the brain you have, and finding ways to make life work for you, not against you.
FAQ:
- Is ADHD a real medical condition?
Yes. ADHD is recognized by major health organizations (APA, WHO) as a neurodevelopmental disorder.
- Can you have ADHD without being hyperactive?
Absolutely. Inattentive ADHD is common, especially in women and girls.
- Can ADHD develop in adulthood?
Symptoms must begin in childhood, but many people are not diagnosed until later in life.
- Is ADHD overdiagnosed?
Data shows underdiagnosis is still a bigger issue, especially in women, minorities, and older adults.
- Is it possible to treat ADHD without medication?
Yes. While medication can help, therapy, coaching, routines, and lifestyle changes also play a major role.
- Is ADHD the same as being easily distracted?
Not quite. ADHD involves deeper challenges in attention regulation, emotional control, and executive functioning.
- What is “masking in ADHD”?
It’s when people hide symptoms to fit in — often at great mental cost. It is mostly common in women and neurodivergent individuals.