The Silent Side Effect: How Antidepressants Affect Sexuality

Depression doesn’t strike evenly. The World Health Organisation estimates that around 4% of the global population is living with depression at any given time — including 6.9% of women and 4.6% of men. That means roughly 1 in 5 women and 1 in 10 men will experience major depressive disorder over a lifetime.
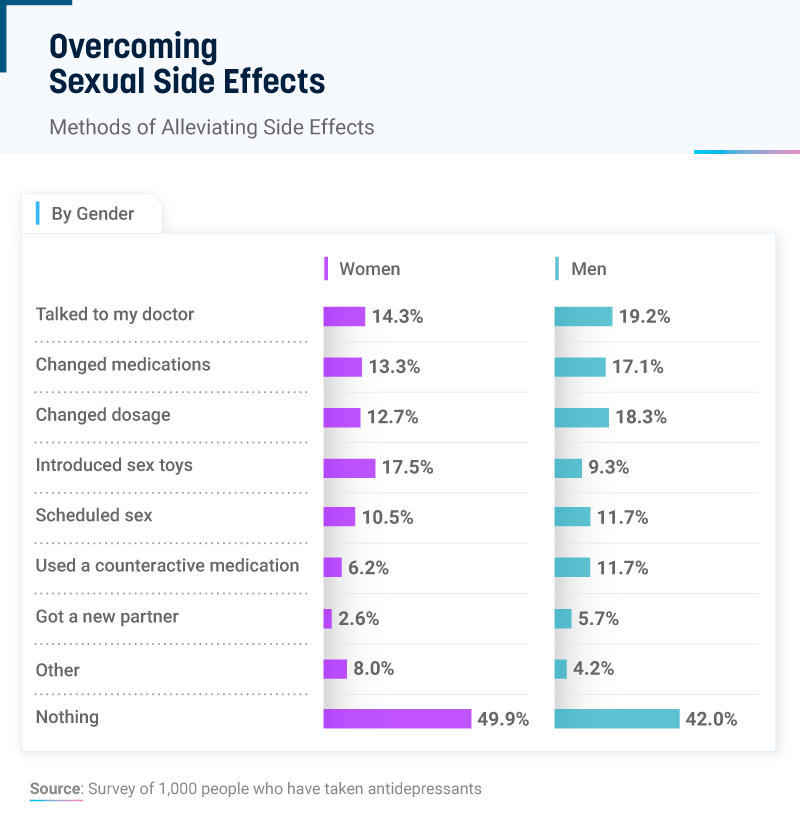
While depression is treatable through medicines, therapy and lifestyle changes, for many, recovery through the use of antidepressant medications comes at a cost that’s rarely talked about in the doctor’s office: a quiet fading of desire, pleasure, or physical response. Sexual dysfunction is one of the most common yet problematic side effects of antidepressant use, and it is one that many prefer to keep secret.
The Hidden Epidemic
Antidepressants are meant to help you feel “normal” again and return colour to a life that’s gone flat. But the medications that alter serotonin-signalling in the brain, often do so at a cost — muting dopamine pathways and flattening feelings, including desire, significantly impacting patients’ quality of life and treatment adherence.
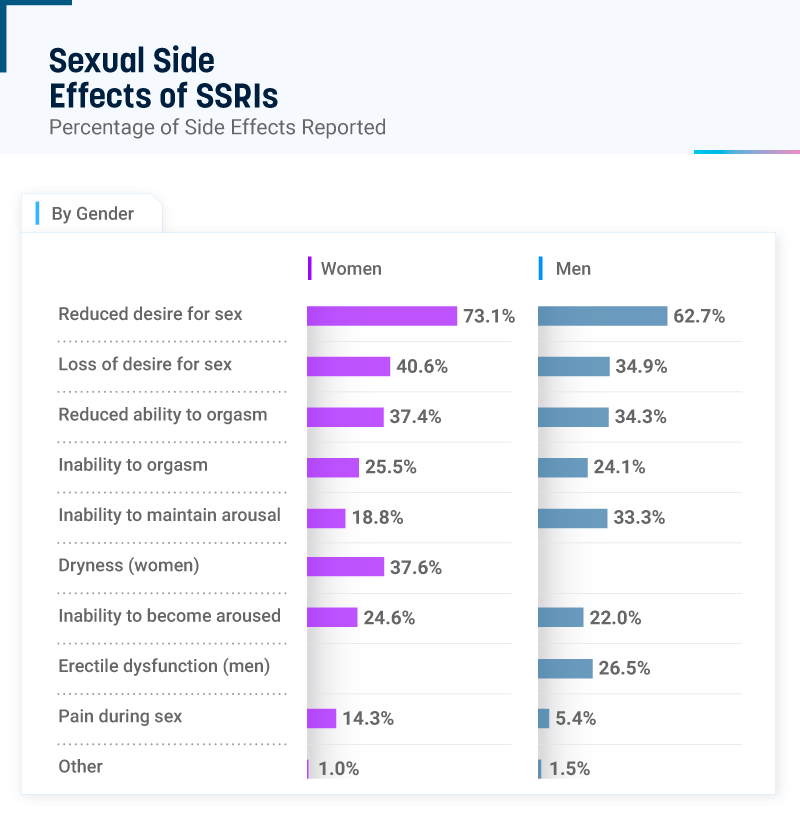
Recent research found that nearly half of outpatients on antidepressants reported sexual side effects. A 2024 meta-analysis of more than 14,000 reports across 21 antidepressant compounds showed that women are disproportionately affected, especially by SSRIs like escitalopram (Lexapro), sertraline (Zoloft), and fluoxetine (Prozac). This blunting isn’t just about libido; it can feel like an inability to feel any sexual sensations at all, quietly rewiring the body’s circuitry. And for many women, whose sense of intimacy is closely linked to emotional connection, the effect can be both disorienting and profoundly isolating.
For some, the sexual side effects don’t fade even after stopping medication — a condition known as post-SSRI sexual dysfunction (PSSD), where loss of arousal and sensation can persist for years or even decades. As a PSSD patient named Rosie Tilli confessed to The Guardian: “My clitoris feels like my elbow now, and there’s nothing I can do to reverse it.”
Facing the Gender Gap
This silence has a cultural component. In clinical conversations, female pleasure still sits in the shadow of male dysfunction. Erectile dysfunction is treated as a medical emergency; women’s loss of desire is often minimised as “psychological” or “secondary.”
For instance, earlier studies suggested men reported these side effects slightly more often, but that possibly reflects more bias rather than biology. Men’s symptoms, like erectile or ejaculatory changes, are easier to identify and discuss, while a fading of desire, muted arousal, or distant orgasms in women often remain unspoken or downplayed.
When Rosie first spoke to her GP about what was happening, she was dismissed as “neurotic.” Her doctor insisted SSRIs couldn’t cause sexual dysfunction and suggested deep breathing instead. What followed was even more devastating. “When I reached out to my local mental health service, I was sectioned and placed in involuntary care,” she recalls. “The psychiatrist said I had a delusional disorder and prescribed antipsychotics. It shattered my trust in ever seeking help again.”
Why Antidepressants Alter Sexual Function
Antidepressants don’t just lift mood — they reshape the brain’s chemistry, and with it, the way the body feels pleasure. Most modern antidepressants, especially selective serotonin reuptake inhibitors (SSRIs) and selective serotonin-norepinephrine reuptake inhibitors (SNRIs), alter serotonin signalling to calm the mind. But when serotonin rises too high, it quiets dopamine and norepinephrine — the neurotransmitters that fuel curiosity, desire, and sexual energy.
Researchers believe this occurs both in the brain and throughout the body, as serotonin influences not only mood but also vascular and nerve function. The result is often a dimming of the erotic pulse: lower libido, muted arousal, delayed orgasm, or loss of genital sensation. These changes can show up within weeks of starting medication — and sometimes linger for as long as the treatment lasts (or even after it’s over).
How High Are the Risks?
These effects aren’t universal and depend significantly on the type of medication. Genetic and physiological differences may also make some people more vulnerable than others.
Drugs that act mainly on serotonin — like SSRIs, SNRIs, and the tricyclic antidepressant clomipramine (Anafranil) — are linked to the highest rates of sexual dysfunction, often affecting up to 70–80% of users. In contrast, non-serotonergic options such as Norepinephrine and Dopamine Reuptake Inhibitors (NDRIs) like bupropion (Wellbutrin) are less likely to cause sexual side effects and may even enhance libido for some.
For many women, switching to these alternatives can make a significant difference. However, they can also bring their own risks — including insomnia, dry mouth, elevated heart rate, and, in rare cases, seizures. The choice often becomes a trade-off: emotional balance on one side, sensual connection on the other.
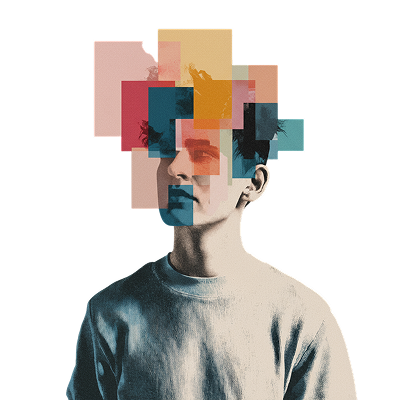
The Emotional Weight of a Muted Body
What patients describe as “sexual dysfunction” may reflect more than a physical side effect — it’s often part of a broader emotional blunting linked to serotonergic overactivity. The result, for many, is a numbing of the body and mind: arousal that never fully ignites, touch that feels distant, emotions that flatten into a muted calm.
For decades, these experiences were minimised or pathologised. A 2016 study reported that 15% of women stopped taking their psychotropic medication because of sexual side effects, yet half never discussed these concerns with their prescriber.
Fortunately, recent research and modern discourse are challenging this stigma, showing that women’s sexual health is closely tied to overall well-being. Positive sexual experiences boost self-esteem, life satisfaction, and reduce anxiety and depression, while sexual dysfunction can contribute to emotional distress and a lower quality of life.
The Road Ahead: What Сan Be Done?
Treatment doesn’t have to mean choosing between mental health and sexual wellbeing. Sexual side effects are common, but they’re not inevitable — and in many cases, reversible. The first step is to identify whether the issue stems from the medication itself or from the underlying depression, which can also suppress desire and arousal in up to half of untreated cases.
If sexual difficulties persist after mood symptoms improve, several evidence-based strategies can help:
- Switching antidepressants: Moving from an SSRI to a drug with fewer sexual side effects — such as bupropion (Wellbutrin), mirtazapine (Remeron), or vortioxetine (Brintellix) — often restores sexual function. Bupropion, which acts on dopamine and norepinephrine rather than serotonin, may even enhance libido and arousal.
- Timing and dosage adjustments: Some people find relief by lowering their dose under medical supervision or adjusting when they take the medication to minimise side effects.
- Psychosexual therapy: Even when the cause is physiological, sexual difficulties can erode confidence, intimacy, and self-image. Therapy — alone or with a partner — helps rebuild communication, manage shame, and reestablish a sense of pleasure and connection.
- Scheduling sex: Some antidepressants cause stronger side effects at certain hours — for instance, within a few hours after taking a dose. If that’s the case, shifting the timing of the medication or planning intimacy can help reduce interference with arousal and orgasm. Always make such adjustments with your doctor’s guidance.
Above all, awareness is essential. When patients are informed about these risks before treatment begins, they’re more likely to recognise early signs, speak up, and work collaboratively with their providers to find a balance between emotional stability and sexual vitality.