Postpartum Rage Doesn’t Mean You’re a Bad Parent. It Means You’re Overloaded

- Postpartum rage affects up to one in four new mothers but often goes unreported.
- It results from hormonal crashes, sleep loss, and lack of social support.
- Strong family and peer support can significantly shorten the recovery period.
- Therapies such as CBT, DBT, IPT, and EMDR have shown effectiveness rates of 70–90%.
- Early recognition and treatment restore emotional balance within 3-6 months.
The baby won’t stop crying. Your pulse spikes, your jaw locks, and suddenly you feel like you might burst. A minute later, guilt hits hard. Nothing is wrong with you. You’re not broken — you’re overloaded.
Studies show that around 1 in 4 new mothers experience intense anger or outbursts after giving birth. Yet 73% of them never mention it to a doctor, fearing judgment or disbelief. This anger, called postpartum rage, isn’t a failure of motherhood. It’s a stress signal from a body that’s healing, sleep-deprived, and flooded with hormonal shifts. Recognising it is the first step toward care, calm, and recovery.
What Is Postpartum Rage
Postpartum rage is a recognised mood disruption that causes episodes of intense anger, frustration, or agitation after giving birth. Mental health experts classify it within perinatal mood and anxiety disorders (PMADs): the same family as postpartum depression and anxiety.
Clinically, it often stems from rapid hormonal shifts, sleep deprivation, and emotional overload during the so-called 4th trimester: the first months when the body, brain, and identity are adjusting to motherhood. Yet for many, it feels less like a diagnosis and more like a loss of control.
Postpartum rage can manifest as sudden, disproportionate bursts of anger that seem impossible to control, followed by guilt, shame, or tears. Many parents describe moments of shouting, slamming doors, or feeling a physical rush of heat and tension through the body. Healthline notes that symptoms can include “struggling to control your temper,” “increased amount of screaming or swearing,” and “physical expressions like punching or throwing things,” often followed by “a flood of emotions immediately afterwards”.
Common emotional and physical signs are:
- Snapping or yelling over small things like spilt milk;
- Clenched jaw, shaking hands, or heat in the chest;
- Racing thoughts, panic, or shame right after an outburst;
- Dwelling on something upsetting or feeling unable to “snap out of it” on your own;
- Exhaustion, guilt, or burnout.
Postpartum rage often appears alongside sleep deprivation, breastfeeding struggles, colic, or unmet expectations of motherhood — everyday stressors that heighten emotional vulnerability. Experts emphasise that this anger does not reflect poor parenting or lack of love. It’s a stress response: a physiological and emotional reaction to hormonal change, exhaustion, and social isolation.
How It Differs from Postpartum Depression
Postpartum rage isn’t a separate diagnosis, but it belongs to the family of perinatal mood and anxiety disorders. These conditions often overlap, and that’s why rage is frequently missed. Anger can hide behind sadness, mask exhaustion, or accompany constant worry. Here’s how they differ — and where they blend:
- Baby blues are short-lived mood changes caused by hormonal shifts after birth. Tearfulness, irritability, and sensitivity are common, but these feelings usually fade within 2 weeks.
- Postpartum depression lasts longer and runs deeper. It brings persistent sadness, guilt, loss of interest or pleasure, emotional numbness, and overwhelming fatigue that interfere with daily life.
- Postpartum anxiety often feels like your mind can’t stop racing — a cycle of dread, panic, and “what ifs.” You may feel constantly on alert, unable to rest or trust that things are okay.
- Postpartum rage is different again: sudden, explosive anger, irritability, or agitation that feels impossible to control, often followed by guilt or shame.
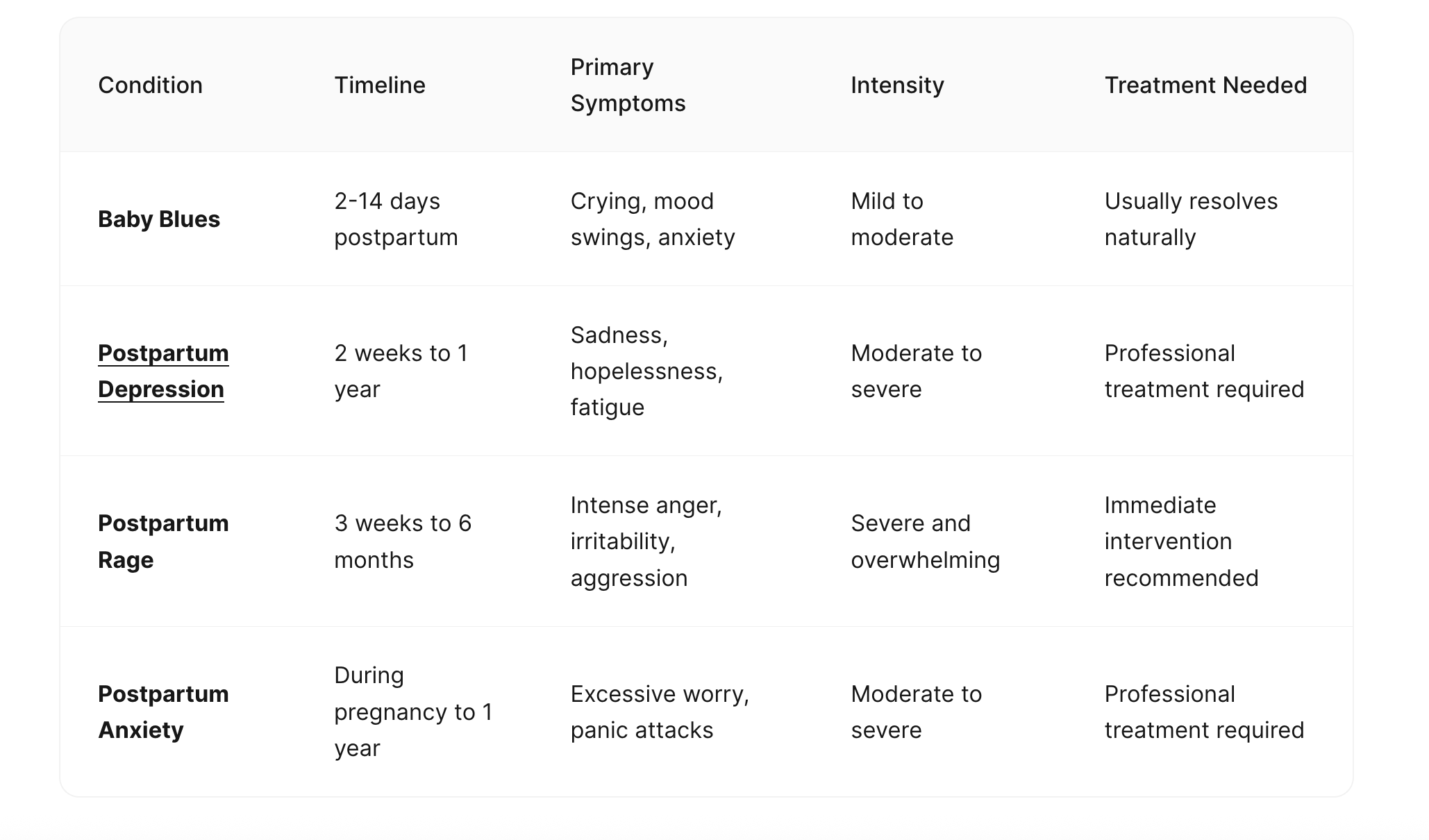
Researchers note that about 50% of mothers who report anger do not meet the criteria for depression, showing that rage can exist on its own or appear alongside other symptoms. Recognising that anger can mask sadness or grow from the same exhaustion helps transform shame into understanding and opens the door to the right kind of help.
Why It Happens: The Science and the System
Postpartum rage is a chain reaction: hormones, neurobiology, exhaustion, identity loss, and isolation feed into one another until the nervous system simply overloads. Researchers describe postpartum rage as both a physiological and social disorder: a reaction that begins in the body’s chemistry but intensifies when new parents face sleep deprivation, limited support, and high caregiving demands.
Hormonal shifts
After birth, estrogen and progesterone levels drop, disrupting serotonin and dopamine — neurotransmitters that regulate mood and impulse control. This hormonal crash can cause irritability, agitation, and emotional volatility even in people with no prior mental health history.
Neurobiology under stress
The amygdala, the brain’s fear and anger centre, becomes hypersensitive in the postpartum period, while cortisol, the stress hormone, remains elevated for weeks. This combination heightens reactivity and makes even minor frustrations feel unbearable.
Sleep deprivation
New parents lose up to 700 hours of sleep in the first year. The lack of REM sleep, crucial for emotional regulation, reduces impulse control by roughly 25–30%, making anger harder to manage.
Identity shift and loss of autonomy
The 4th trimester brings a psychological transition: autonomy shrinks, personal time disappears, and constant caregiving replaces self-agency. Mothers describe feeling “trapped in competence” and expected to do everything without complaint. That dissonance fuels resentment and rage.
Social isolation
For centuries, large families and communities shared caregiving. Today, thousands of parents navigate newborn life alone, far from family, community, or without maternity leave. Lack of support correlates with higher cortisol levels, depressive symptoms, and episodes of uncontrolled anger.
Trauma and perfectionism
Those with a history of depression, anxiety, or trauma are 60–85% more likely to experience postpartum anger. So are parents who hold rigid standards for themselves, believing good mothers never lose control.
Taken together, postpartum rage is a symptom of systemic burnout. The single most protective factor across studies is social and emotional support: when mothers are heard, helped, and rested, their anger tends to calm down.
Who Feels Postpartum Rage Most
Postpartum rage can affect any new parent, but some are more at risk because of how biological and social stressors intersect.
- Previous depression or anxiety
Those with a mental health history are around 60% more likely to develop postpartum anger or irritability. Their nervous systems are already sensitised to stress. - Traumatic or complicated birth
Emergency cesareans, prolonged labour, or medical trauma raise the risk by up to 85%, often turning fear and helplessness into anger. - Economic and social vulnerability
Low income, single parenthood, or teenage motherhood can double or even triple the risk. Financial strain and limited childcare amplify stress. - Sleep deprivation and medical stressors
Poor sleep and NICU stays (Neonatal Intensive Care Unit) directly predict higher irritability and emotional volatility. - Lack of partner or community support
Isolation consistently worsens postpartum anger. Social support acts as a strong emotional buffer. - Cultural pressure to stay “grateful”
Many mothers feel guilty for expressing frustration, fearing judgment or failure. Suppressed anger then turns inward as shame.
Partners and fathers can experience similar symptoms: irritability, fatigue, withdrawal, showing that postpartum rage is a human response to chronic stress, determined not only by gender.
The Hidden Costs of Anger
When postpartum rage goes unrecognised, it ripples through the family system. Constant tension and guilt can leave parents feeling drained, defensive, and disconnected. The body stays on alert, even when there’s no real threat, leading to exhaustion, headaches, and emotional burnout.
In relationships, postpartum rage frequently shows up as communication breakdowns. Exhausted parents lash out over small triggers, like an undone chore or a crying baby, because it represents a buildup of unmet needs. Partners, unsure how to respond, may retreat, creating a cycle of anger, guilt, and withdrawal that reinforces distance. Over time, the household becomes quieter, colder, more fragile. Studies also note that persistent irritability can create emotional distance from the baby because chronic stress suppresses empathy and bonding.
Children also pick up on this tension. Even infants sense changes in tone and energy; older siblings may respond with confusion or clinginess. As COPE notes, postpartum frustration and anger can be directed toward “children, family members and ourselves,” which understandably erodes connection. When the anger isn’t named, the emotional distance widens. Parents report feeling “like roommates, not partners,” and describe the shame of not living up to the idealised image of calm, grateful parenthood.
Encouragingly, most couples who address rage recover closeness and empathy once both partners understand that anger signals exhaustion. 87% of mothers regain full emotional connection with their child after receiving therapy, and those who include their partners in therapy improve faster. The same study found that improvement typically begins within 6 to 8 weeks of consistent treatment. Early recognition and open conversation with a partner, doctor, or therapist can prevent anger from hardening into burnout and help restore stability.
Why Postpartum Anger Goes Unseen
Anger is one of the last taboos of motherhood. While sadness and anxiety are now openly discussed, rage still feels forbidden as something unfeminine, even dangerous. Many mothers describe being more afraid of judgment than of their own anger.
Postpartum checkups rarely make space for these feelings. Most screening tools, like the Edinburgh Postnatal Depression Scale (example), are designed to detect sadness or hopelessness but not fury or emotional overload. As a result, parents who are screaming into pillows rather than crying in silence often go unnoticed by healthcare providers.
Experts are now urging for change. Mental health advocates and perinatal psychiatrists are pushing to include anger in standard postpartum screenings, arguing that it’s one of the most overlooked symptoms of perinatal mood disorders. Acknowledging anger doesn’t make motherhood darker, but it makes it more honest.
Calming Practices to Regain Control
When anger hits, reasoning collapses. The aim is to take a break. Even a few seconds of calm can interrupt the body’s stress cascade. These short, research-backed techniques help the nervous system move from fight-or-flight toward regulation.
The STOP method
Mindfulness trainings propose to Step away, Take a breath, Observe, and Proceed mindfully. This grounding STOP sequence interrupts impulsive reactions and activates the prefrontal cortex, the brain’s decision centre, helping emotions settle before action.
The 4-7-8 breath
Breathe in for 4 seconds, hold for 7, exhale for 8. Developed by Dr. Andrew Weil and supported by psychophysiological studies, this breathing rhythm lowers blood pressure and cortisol, helping the body exit acute stress faster.
Sensory grounding
Running cold water over your wrists or using the 5-4-3-2-1 method (five things you see, four you can touch, three you hear, two you smell, one you taste) engages sensory input to deactivate the amygdala’s alarm response. Both techniques are used in cognitive-behavioural and trauma-informed therapy for emotional regulation.
Journaling triggers
Recording what happens before, during, and after an outburst helps identify patterns like lack of sleep or overstimulation, turning vague emotion into observable data. Self-monitoring is a standard component of cognitive-behavioural therapy for mood regulation.
Physical release
Anger produces a measurable spike in adrenaline and muscle tension. Releasing it through movement — walking, stretching, shaking out your hands — restores physiological equilibrium and reduces rumination.
Proven Therapies for Postpartum Rage
Self-soothing tools can help you survive the moment. Nevertheless, real healing requires structured treatment: therapy, support, and sometimes medication.
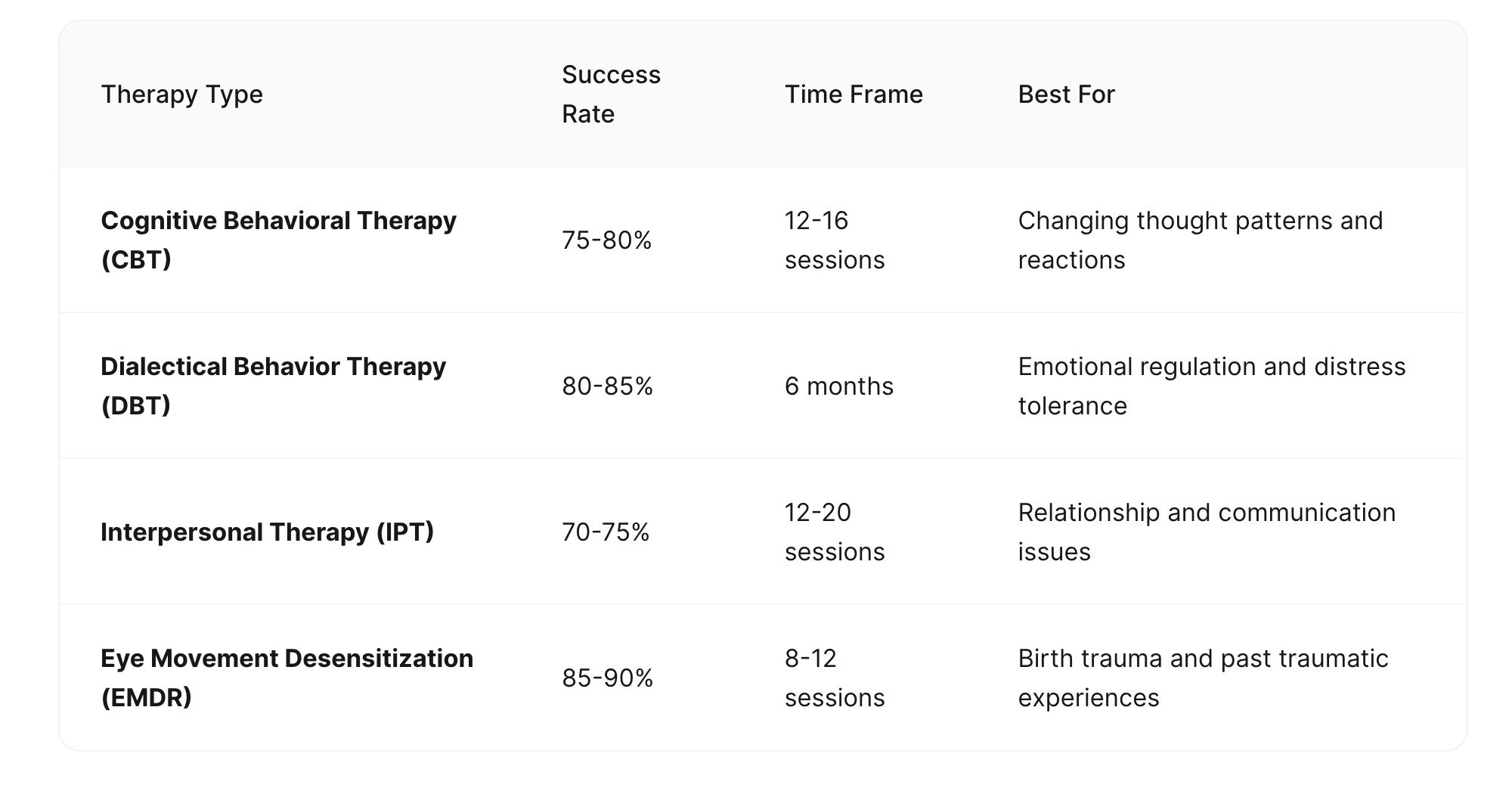
Psychotherapy works — and fast
Cognitive Behavioural Therapy (CBT), Dialectical Behaviour Therapy (DBT), Eye Movement Desensitisation and Reprocessing (EMDR), and Interpersonal Therapy (IPT) have shown 75–90% effectiveness in reducing anger, anxiety, and depressive symptoms when practised consistently.
CBT helps identify and reframe the thoughts that feed rage (“I’m failing” to “I’m overwhelmed and need rest”). DBT adds emotion-regulation tools and mindfulness. IPT focuses on rebuilding support and communication. EMDR can be especially useful for those whose anger roots in birth trauma.
Medication
For moderate to severe symptoms, psychiatrists may prescribe SSRIs or SNRIs, such as sertraline, fluoxetine, or venlafaxine, which are considered safe while breastfeeding. These medications stabilise mood by balancing serotonin and norepinephrine levels, reducing reactivity and emotional volatility.
Connection
Peer and group therapy, including programs through Postpartum Support International (PSI), significantly reduces shame and loneliness. Hearing “me too” reframes rage as a shared experience. Group-based support is associated with lower relapse rates and faster emotional recovery.
If you bring only one thing to your next postpartum checkup, let it be this: name the anger. Don’t minimise it as stress or sadness. Naming it out loud helps your doctor recognise it for what it is and form a relevant treatment plan.
How Partners and Families Shape Recovery
Postpartum recovery isn’t a solo project. Across studies, one factor stands out as the most protective against postpartum anger and depression: social support. Emotional regulation improves when mothers and partners feel seen and helped, and recovery accelerates.
Why connection matters
Support provides emotional and biological comfort. Oxytocin, released through touch, conversation, and care, counteracts the stress hormone cortisol. In other words, every kind text, shared meal, or ten-minute break is a small chemical act of healing. Parents with high perceived support experience lower anger, shorter recovery, and better bonding with their child.
Ways to rebuild your support system
- Share the load: split night shifts, chores, or feedings with your partner. Practical help matters more than words.
- Join a community. Online groups offer validation, education, and peer empathy anytime, anywhere.
- Create a “support map.” Identify 6 people: 3 for practical help (groceries, childcare, chores), 2 for emotional support, and 1 emergency contact for crises. Seeing names written down helps the abstract become real.
For partners, family, and friends
Your response matters as much as any treatment plan if someone you love is struggling. Here are some psychotherapists’ recos:
- Listen without trying to solve everything;
- Validate what you hear (“That sounds really hard”);
- Step in with concrete help — laundry, food, time for rest;
- Check in consistently, not just once;
- Don’t minimise or explain away the anger;
- Don’t say “just calm down” or “other moms handle it fine.”
- As therapists often say, “Validate first, fix later.”
Sometimes, the most powerful thing you can do for a parent in pain is simply to stay. Quietly, consistently, and without judgment.
What Works in Recovery: Evidence & Everyday Care
Postpartum rage is a reversible neurobiological and psychosocial condition. When recognised early and treated systematically, outcomes are consistently positive. Clinical reviews show that most patients regain baseline emotional regulation within 3 to 6 months with structured therapy, medical follow-up, and adequate social support.
The mechanisms of improvement are well studied:
- Psychotherapy (CBT, DBT, IPT) retrains the brain’s response to stress by restoring balance between the prefrontal cortex and amygdala.
- Pharmacological support, when indicated, corrects serotonin and norepinephrine imbalance.
- Social support reduces cortisol levels and increases adherence to treatment plans.
- The most effective interventions combine emotional validation with logistical relief: rest, practical help, and consistent follow-up with qualified providers.
The data are unambiguous: early identification and coordinated care improve recovery speed and prevent chronic strain in family systems. Recognising postpartum rage as a treatable response to cumulative stress is the first step toward mindful stability.
FAQ
- What causes postpartum rage?
It develops through a combination of hormonal changes, chronic sleep deprivation, emotional overload, and lack of social support. The crash of estrogen and progesterone after birth disrupts serotonin and dopamine, heightening reactivity and frustration.
- How common is postpartum rage?
Research estimates that up to 1 in 4 new mothers experience intense anger or outbursts during the first year after giving birth — though most never report it to a doctor.
- How long does postpartum rage last?
When left untreated, symptoms can persist for several months or longer. Most parents regain emotional stability within 3 to 6 months with therapy and consistent support.
- Is postpartum rage the same as postpartum depression?
No. Rage often coexists with depression or anxiety, but can appear on its own. Depression is marked by sadness and loss of interest; rage shows as sudden anger, irritability, and guilt.
- Can partners or fathers experience it too?
Yes. Partners can develop similar symptoms: irritability, fatigue, and emotional withdrawal, due to sleep loss, stress, and the overall strain of caregiving.
- When should someone seek professional help?
If anger feels uncontrollable, interferes with relationships, or leads to guilt and isolation, it’s time to consult a GP, OB-GYN, or perinatal mental health specialist. Early treatment prevents escalation and speeds recovery.
- What are the best evidence-based treatments?
Therapies like CBT, DBT, IPT, and EMDR show 70–90% success rates. In moderate to severe cases, antidepressants such as sertraline, fluoxetine, or venlafaxine may be prescribed safely during breastfeeding.