What Is Ibogaine and How Does It Work? From Plant to Powerful Therapy

Once a sacred root in Central Africa, ibogaine is now at the centre of modern psychedelic science. Extracted from the Tabernanthe iboga plant, this psychoactive compound is being studied worldwide for its potential to treat addiction, depression, and PTSD. While ibogaine remains illegal in the United States and carries safety concerns, new clinical trials are underway in Mexico, Europe, and beyond. With governments now investing in large-scale research — including a $50 million program in Texas — ibogaine has moved from underground ceremonies into mainstream medical debate.
What Is Ibogaine and Where Does It Come From
Ibogaine is a naturally occurring alkaloid found in the root bark of the Tabernanthe iboga shrub, a rainforest plant native to Central and West Africa. For centuries, it has been central to Bwiti ceremonies in Gabon and Cameroon, where it was used as a sacrament in initiation rituals and healing practices. Unlike classic psychedelics such as psilocybin or LSD, ibogaine is often described as a “oneirogenic” — a substance that produces intense, dream-like visions combined with hours of deep introspection.
Western science first became interested in ibogaine in the early 20th century, when French explorers documented its psychoactive properties. In the 1960s, American researcher Howard Lotsof reported that ibogaine could interrupt heroin dependence, sparking decades of underground use and, eventually, formal clinical studies.
Today, ibogaine is being tested far beyond its ritual roots. Researchers are exploring its potential to ease drug withdrawal, reduce cravings, and even support recovery from depression, PTSD, and traumatic brain injury. While the therapy remains experimental, it has transitioned from secret ceremonies to modern high-end retreats and clinical trials.

Mental Conditions Ibogaine Might Help With
Researchers have begun to map out where ibogaine shows the most promise. From addiction recovery to mental health, the compound appears to influence both the body’s withdrawal processes and the mind’s ability to reset entrenched patterns.
Substance Use Disorders
Opioid Use Disorder (OUD)
Ibogaine first gained attention for its ability to interrupt opioid dependence. Early observational studies suggest that a single session can ease withdrawal symptoms and sharply reduce cravings, often described by patients as a “reset”.
Alcohol Use Disorder (AUD)
In animal studies, ibogaine blocked alcohol-seeking behaviour and reduced relapse risk. Small clinical reports suggest similar effects in humans, although larger trials are still required.
Stimulant Use Disorder (SUD) & Nicotine Cravings
Early data indicate that ibogaine and its metabolite noribogaine may dampen the rewarding effects of cocaine, methamphetamine, and nicotine. The mechanisms are still being investigated, but they likely involve nicotinic acetylcholine receptors.
Mental Health
Depression
Small-scale studies and case reports suggest ibogaine may benefit treatment-resistant depression. Patients often describe a lasting lift in mood following therapy, though controlled trials remain scarce.
PTSD and Traumatic Brain Injury
New research from Stanford and Nature Medicine showed that veterans with PTSD and traumatic brain injury experienced dramatic symptom relief after ibogaine therapy (with magnesium — to protect the heart), including improvements in mood, memory, and impulse control.
Reported Symptom Relief
Beyond specific diagnoses, people who have undergone ibogaine therapy often report distinctive benefits:
- Immediate effects: reduced withdrawal intensity, suppressed cravings, vivid autobiographical visions that help reframe past experiences.
- Longer-term effects: improved emotional balance, stronger impulse control, reduced relapse risk, and, in some cases, lasting improvements in quality of life.
In summary, ibogaine shows the most substantial promise in cases of substance use disorders where standard treatments often fall short. Early evidence also points to potential benefits for treatment-resistant depression, PTSD, and traumatic brain injury. What unites these conditions is ibogaine’s ability to interrupt destructive cycles, reduce cravings, and create space for long-term recovery when paired with proper medical care and follow-up support.
How Ibogaine Rewires Neural Pathways
Scientists often describe ibogaine as a “multi-target” medicine, because it doesn’t act on just one brain receptor. Instead, it targets several key systems simultaneously — including nicotinic acetylcholine receptors, NMDA receptors, serotonin pathways, and kappa-opioid receptors.
By working across these networks, ibogaine seems to reset dopamine circuits that drive reward and craving, the very loops that keep addictions locked in place. At the same time, both ibogaine and its metabolite noribogaine boost levels of neurotrophic factors like BDNF and GDNF — proteins that help brain cells grow new connections and repair old ones. This increase in neuroplasticity may explain why some people feel lasting changes long after a single session.
In simple terms, ibogaine works a bit like pressing several reset buttons in the brain at once. This “double action” — interrupting old loops and encouraging fresh ones — may be the reason for long-term improvements after just one session.
Researchers are also studying safer analogues such as 18-MC (18-methoxycoronaridine), which aim to keep these anti-addictive effects without the intense psychedelic visions or cardiac risks of ibogaine.
Ibogaine Therapy Protocols
Ibogaine treatment isn’t a casual experience — it’s a carefully structured program designed to maximise benefits and minimise risks. Most clinics begin with a medical screening, which typically includes an ECG to assess heart rhythm, laboratory tests for liver and kidney function, and a review of current medications. Only people who pass this screening move forward, since ibogaine can interact with other drugs and stress the heart.
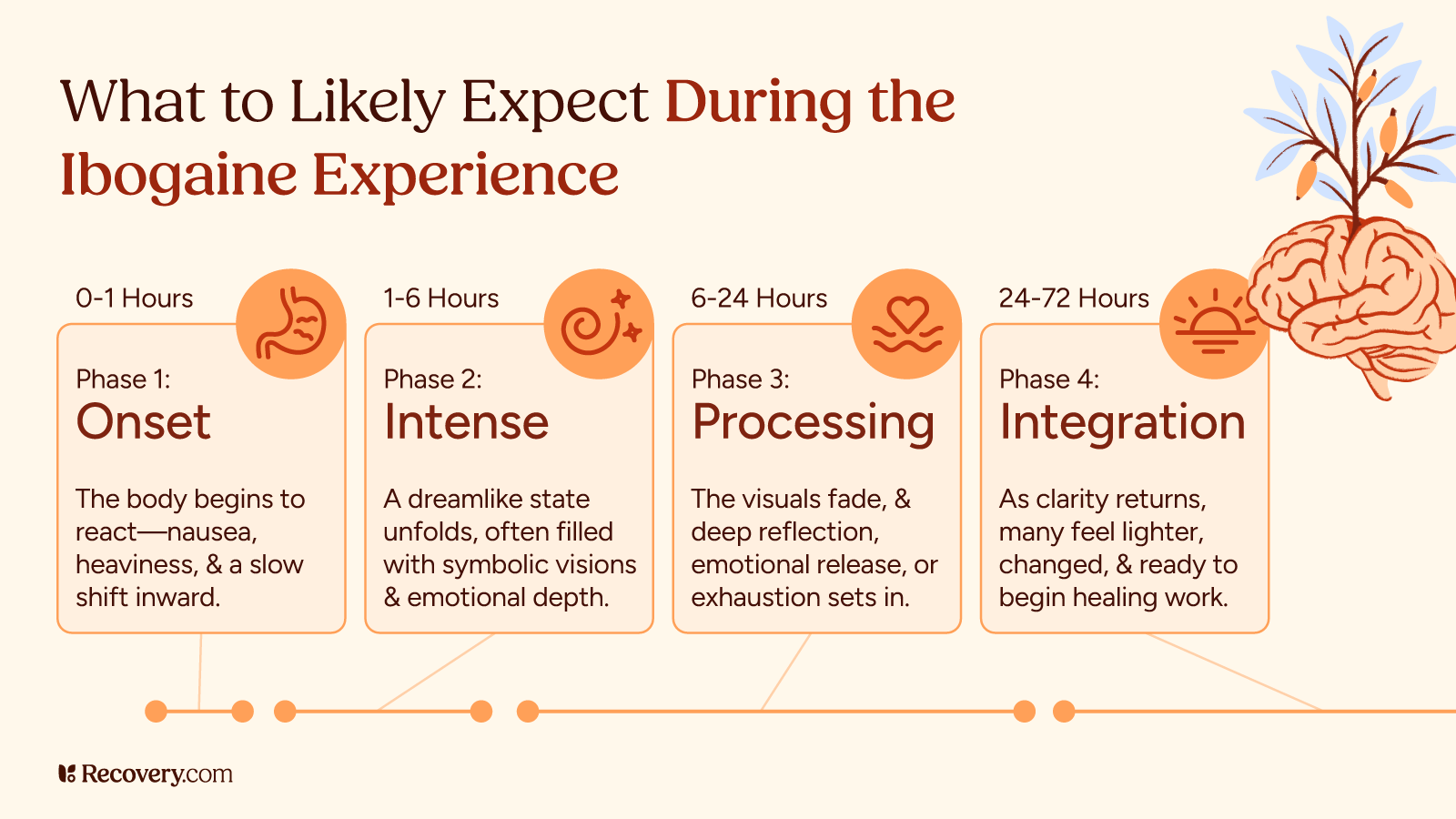
The core of treatment is a “flood dose” of ibogaine, given under constant medical monitoring. The psychoactive journey itself can last 12–24 hours and often brings intense, dream-like visions mixed with long periods of reflection. Patients typically spend the next few days resting, rehydrating, and gradually regaining strength.
After the acute phase, many programs emphasise integration therapy — counselling sessions or group support that help people make sense of what they experienced and apply it in daily life. This step is considered crucial, since the insights from ibogaine need to be anchored in real-world changes.
It’s essential to keep in mind that ibogaine can cause a range of side effects. Common ones include nausea, vomiting, sleeplessness, loss of coordination, and emotional swings. Some people also report muscle tremors or vivid, sometimes unsettling visions. More serious risks involve heart rhythm disturbances (QT prolongation). That’s why experts stress: ibogaine should only ever be administered in clinics with proper safeguards, not in DIY settings.
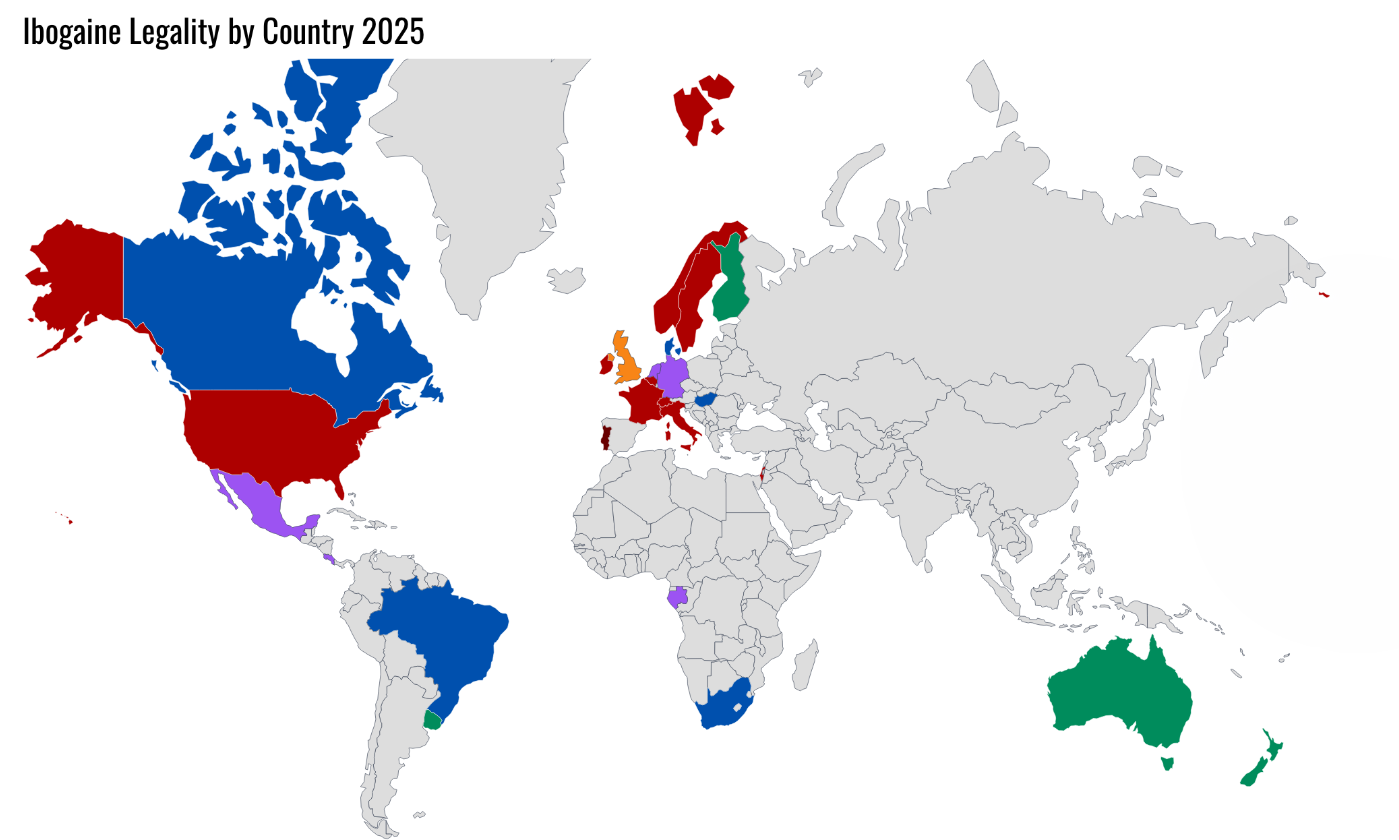
Ibogaine Legal Status
Although ibogaine is gaining attention in neuroscience and clinical studies, its legal status varies widely around the world. In some countries, clinics operate openly; in others, ibogaine is tightly controlled or outright banned. This patchwork of laws shapes not only who can access treatment, but also how quickly formal research can move forward.
🇵🇹 Portugal. Since 2001, Portugal has decriminalised the use of all drugs, shifting the focus from punishment to public health. This policy includes ibogaine, which means that possession and therapeutic use are not criminal offences. This status has allowed some clinics to explore its use in treating addiction under medical supervision.
🇳🇱 Netherlands. The Netherlands has become one of Europe’s key destinations for ibogaine therapy. Ibogaine itself is not listed as a controlled substance under Dutch narcotics law, which makes it legal for specialised clinics to operate. Several ibogaine treatment centres have been established, serving international patients seeking medically supervised programs.
🇩🇪 Germany. Here, ibogaine is listed as a controlled substance under the German Narcotics Act (BtMG). It cannot be prescribed or used in clinics, though researchers have shown growing academic interest in its potential.
🇺🇸 United States. Ibogaine is classified as a Schedule I controlled substance under the Controlled Substances Act, which makes clinical use illegal. Research is allowed only under strict federal approval. Still, momentum is building: in 2025, Texas passed Senate Bill 2308, approving $50 million to fund ibogaine research for addiction and PTSD.
🇨🇦 Canada. Since 2017, ibogaine has been included on Canada’s Prescription Drug List. This means patients can only access it legally through the Special Access Program, which grants physicians approval on a case-by-case basis.
🇲🇽 Mexico. Ibogaine is not formally scheduled under federal law, which allows private clinics to operate openly. This legal grey zone has turned Mexico into one of the leading international destinations for ibogaine therapy.
🇧🇷 Brazil: In 2016, the state of São Paulo legalised ibogaine for prescription use in hospital settings. Brazilian medical authorities are recognising its potential in the treatment of addiction recovery, and ibogaine is allowed for administration under clinical supervision.
Who Is Driving Ibogaine Therapy Research
Beyond governments, non-profits and biotech firms are pushing the field forward. The Multidisciplinary Association for Psychedelic Studies (MAPS) has long advocated for ibogaine research and policy reform. Meanwhile, biotech companies like MindMed are developing ibogaine analogues such as 18-MC, designed to keep anti-addictive effects while reducing psychedelic intensity and cardiac risks.
On the clinical side, treatment providers such as Beond Ibogaine in Mexico are shaping best practices by combining ibogaine therapy with medical monitoring and structured integration programs, offering an early model of how future evidence-based clinics may look.
Read More:
The Courage to Heal: A Conversation With Tom Feegel of Beond Ibogaine Treatment Center
Ibogaine has moved from ritual use to the frontiers of medical research. Studies point to real potential in breaking addiction cycles and easing mental health burdens, but safety concerns remain the main barrier. With larger clinical trials now underway, the question is not whether ibogaine can change lives — but whether science can confirm it is safe enough to do so.
FAQ
- What is ibogaine, in a nutshell?
Ibogaine is a psychoactive alkaloid derived from the Tabernanthe iboga shrub, traditionally used in Central African rituals. Today, it is being studied as an experimental therapy for substance use disorders, treatment-resistant depression, PTSD, and traumatic brain injury.
- How does ibogaine therapy work?
Ibogaine interacts with multiple brain systems, resetting dopamine pathways linked to addiction and boosting neuroplasticity, which may explain lasting effects after one session.
- How is ibogaine different from other psychedelics used in therapy?
Unlike psilocybin or LSD, ibogaine is often described as a “oneirogenic,” meaning it produces long, dream-like visions combined with hours of deep introspection. It also acts on a broader range of brain receptors at once, which may explain its unique ability to reduce cravings.
- Is ibogaine legal?
Ibogaine is decriminalised in Portugal and the Netherlands. Several modern clinics operate in Mexico and Brazil. In Canada, access is possible through the Special Access Program. In most countries, ibogaine is controlled and only allowed for research purposes.
- What conditions might ibogaine help with?
Research suggests ibogaine may help with opioid, alcohol, and stimulant addiction, as well as treatment-resistant depression, PTSD, and brain injury recovery.