“This Is Medicine”: The Fight to Bring Medical Cannabis Into the NHS

Medical cannabis — an umbrella term for THC and CBD-based products that differ in their effects and clinical uses — has been legal (but tightly controlled) in the UK since 2018. Yet doctors are hesitant to prescribe the potentially beneficial treatment, with only a handful of patients receiving NHS prescriptions.
A 2022 survey revealed that an estimated 1.8 million adults in the UK self-medicate with illicit cannabis. However, data suggests that by the end of 2025, around 80,000 people will be accessing cannabis medicine through the legal route.
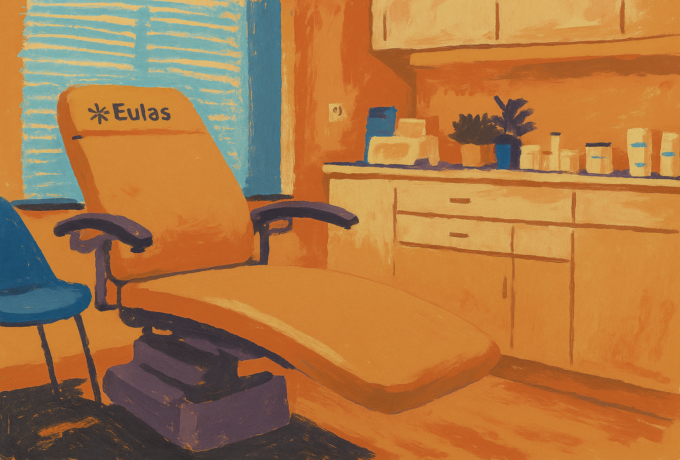
Currently, the large majority of the prescriptions are accessed through private clinics.
Professor of neurology and medical cannabis expert, Mike Barnes, says that barriers to NHS prescribing need to be addressed, including improved education for healthcare professionals, a better NHS model, and the removal of political obstacles.
Clark French, founder of the United Patients Alliance which has been campaigning for patient access to medical cannabis since 2011, says patients are a central force for this change.
“Without advocacy, progress stalls. Industry and regulatory improvements must be patient-focused,” says French.
“Cannabis has enormous potential as a medicine, but barriers around education, affordability, quality, and regulation limit its use.”
Barriers, Bureaucracy, and Stigma Around Medical Cannabis
Since 2018, cannabis-based medicinal products (CBMPs) have been categorised in Schedule 2 under the Misuse of Drugs Act 1971, as they contain the psychoactive compound THC, among other cannabinoids, meaning only specialists can prescribe the medicine.
Products that contain only CBD — a non-psychoactive cannabinoid — are sold over-the-counter and are regulated by the Foods Standards Agency.
However, the UK’s National Institute For Health And Care Excellence (NICE) only recommends a select number of CBMPs for refractory chemotherapy nausea, MS spasticity, severe epilepsy and neuropathic pain. Other cannabis medicines are classed as unlicensed medicines, falling under ‘specials’ regulations.
In order to receive an NHS prescription, patients must first have tried at least two other conventional treatments that did not work.
Any cannabis prescription must then be issued by a specialist prescriber that is registered with the General Medical Council (GMC) register, who must also apply for NHS funding for the medicine.
In an attempt to relax these rules, a parliamentary bill called the Medical Cannabis Access Act, was put forward to parliament in 2022 that would have allowed GPs to prescribe the medicine. The bill was unsuccessful.
This framework can make it difficult for patients to access medical cannabis, with fewer than five prescriptions issued by the NHS as of 2024.
Choose the Type of Support That Matches Your Need
Barnes says that this current process for prescribing is “not unreasonable in principle”, but in practice, is extremely difficult to navigate.
He notes that medical bodies such as The Royal College of Psychiatrists, the Royal College of Physicians, and the British Paediatric Neurology Association, remain largely opposed to the medicine.
Professional bodies do emphasize limited evidence, but not an absolute ban.
NICE guidance supports cannabis-based products for defined indications such as intractable nausea and vomiting, refractory epilepsy, MS spasticity, and chronic neuropathic pain. Additionally, the British Paediatric Neurology Association now recommends pure CBD as first-line for severe childhood epilepsy, and advises against using THC-containing or artisanal oils in children.
Barnes says the reason for this caution lies in the perceived lack of evidence based on the limited number of traditional clinical trials around medical cannabis.
“That’s not really accurate,” says Barnes.
“If you look beyond pharmaceutical-style clinical trials and examine real-world evidence, there’s actually a lot of data supporting the use of medical cannabis.”
For example, data from the patient registry, Project T21, indicates that patients with conditions such as chronic pain, anxiety and PTSD, saw significant improvements in their symptoms and overall quality of life.
Additionally, patients enrolled on the UK Medical Cannabis Registry, which collates outcomes of medical cannabis prescribing, have seen significant improvements in PTSD symptoms, anxiety and sleep quality. However, results from these projects need to be replicated in clinical trials.
Barnes highlights that the problem is that cannabis doesn’t fit the pharmaceutical model as it is a botanical product, and not a single-molecule drug. This can make investigations, including blinding, placebo matching, and understanding the mechanism of action, difficult to carry out, for example.
Adding to this, the historic stigma against cannabis still runs deep — contributing to the hesitancy of medical professionals to prescribe.
Barnes highlights that because cannabis has long been associated with recreational use, currently, many medical professionals assume it cannot have medical value.
Additionally, he highlights that healthcare professionals struggle to accept a medicine that can be prescribed for multiple different conditions.
“The medical profession is used to drugs that target one specific issue, for example, one antibiotic for one infection, one blood pressure drug for one condition.
“There’s also a misconception that because cannabis is touted to help with a wide range of conditions from pain to epilepsy, it must be “too good to be true.” That’s simply a misunderstanding of how it works,” says Barnes.
While many patients indeed report broad symptom relief, high-quality evidence exists only for certain conditions — which is why NICE recommends cannabis-based medicines only for specific indications.
Medical Cannabis Education and Training
This stigma and lack of education is one of the biggest challenges to overcome.
Currently, the entire endocannabinoid system is not taught in health education courses or medical schools in the UK, contributing to the lack of understanding from healthcare professionals.
Barnes, who is also the founder of the Medical Cannabis Clinicians Society (MCCS), is now working to change this by offering courses through MCCS to educate clinicians on cannabis.
“We’re approaching medical schools to ask if we can at least include one lecture on the subject — not a full course, just a starting point,” says Barnes.
“That project is in its early stages, but it’s an important step.”
For doctors already qualified, the MCCS also runs training days, publishes guidelines and booklets, and offers monthly teaching courses, having taught over 500 clinicians so far.
“The goal isn’t to make everyone prescribe cannabis, but to ensure they’re informed enough to make a sensible decision rather than rejecting it out of ignorance,” says Barnes.
From a patient perspective, French says that doctors need to listen to their patients.
“Patients often know their conditions best. Medical expertise is vital, but trust needs to be two-way, especially in cannabis,” French says.
Product Quality, Regulation, and Cost
Patients report experiencing problems with the quality of some of the cannabis products they receive.
Medical cannabis products come into the country through the Medicines and Healthcare products Regulatory Agency (MHRA), and while there are some UK cultivators, the majority of products are imported.
“It’s ultimately the MHRA’s responsibility to ensure that what enters the country meets GMP [good manufacturing practice] standards,” says Barnes.
“Clinics prescribe in good faith, but sometimes a bad batch slips through. That’s part of dealing with a natural, botanical product, occasionally, something goes wrong. When that happens, the pharmacy or distributor should remove the product immediately.”
Such an incident occurred in 2021, when products found to be contaminated with mold were recalled.
Cannabis could become a first-line treatment for certain conditions such as chronic pain, anxiety disorders, and PTSD.
Quality control has improved significantly in recent years, and Barnes explains that the MCCS has also developed Best Practice Guidelines outlining how clinics should operate.
These include checks for contraindications, peer-review panels for high-THC prescriptions, and proper follow-up procedures.
Clinics, which are regulated by the Care Quality Commission (CQC), will be asked to sign and commit to the guidelines, and those that sign will be listed as adhering to good practice standards.
“We’re essentially trying to help the industry self-regulate,” Barnes explains.
Patients also highlight cost as a major barrier. The average cost is around £4 to £6 per gramme and patients sometimes pay hundreds of pounds per month. While there are low-income schemes available, these costs affect equity and patient safety – driving people to continue using the black market.
Cannabis has enormous potential as a medicine, but barriers around education, affordability, quality, and regulation limit its use.
Barnes highlights that, while these costs have seen dramatic progress compared to a few years ago, ultimately he believes that “it shouldn’t cost anything for patients who qualify, it should be free on the NHS.”
“If the NHS started prescribing, producers would sell far greater volumes at lower prices — which would still be commercially viable and good for patients,” adds Barnes.
The UK has seen similar models before. Barnes explains in his previous work in brain injury rehabilitation, the NHS previously initially didn’t provide services but over time began subcontracting to private providers, reimbursing the providers for care.
“I suspect the same will happen here, that NHS prescriptions will initially be handled by private cannabis clinics, and paid for by the NHS,” he says.
NHS Reform
Prescribing cannabis can be a complex task with a need for specialist expertise.
Barnes says that providing dedicated cannabis specialists and trained prescribers can help improve access to the medicine.
The MCCS has been actively working toward this goal through its training and education, and today there are 150 doctors in the UK who can legally prescribe cannabis.
“Ideally there would be a formalised specialist pathway such as a cannabis medicine diploma or recognised clinical subspecialty, similar to addiction psychiatry or pain medicine,” says Barnes.
“That would professionalise the field and reassure both the NHS and the public that this is serious, evidence-based medicine.”
To improve confidence in cannabis medicines, the MCCS training programme and Project Twenty21, are both helping build this evidence base.
Currently, National Institute for Health and Care Excellence (NICE) guidelines only support the use of two licensed cannabis-based medicines. Other cannabis medicines such as flowers and oils are unlicensed but still legally prescribable, creating confusion among doctors.
The MCCS has proposed that NICE develop a separate botanical evidence framework, suggesting that instead of relying solely on double-blind placebo trials, cannabis could be assessed using RWE.
UK registry data and cohort studies provide some support for this approach. An analysis of UK Medical Cannabis Registry participants reported reductions in pain scores, anxiety and sleep problems after three to six months of treatment.
And while ‘real-world’ reports are encouraging, they are not yet confirmed by large trials.
However, the UK government is now developing regulatory frameworks and guidance around RWE to complement clinical trials, and has now established its RWE Scientific Dialogue Programme.
“The biggest step forward would be for NICE to formally acknowledge that cannabis doesn’t fit the conventional drug approval model and create a parallel evidence pathway for plant-based medicines,” Barnes says.
“Cannabis could then become a first-line treatment for certain conditions such as chronic pain, anxiety disorders, and PTSD, where it’s already shown strong evidence in real-world settings.”
The Future for Medical Cannabis as Healthcare
For meaningful reform to happen within the NHS, Barnes says there needs to be political will behind the drive to create a system of infrastructure that can deliver cannabis medicine effectively.
“Change will come from data, persistence, and public pressure,” says Barnes.
“The 2018 legislation was a step forward, but it was passed without proper infrastructure or follow-up policy.”
Since then, the topic of medical cannabis has been largely avoided by the government — with debates on the matter filibustered in parliament, blocking a bill to improve access for patients.
What is holding the industry back is the current scheduling of medical cannabis, says French, which is currently a Schedule Two drug.
“It’s in the wrong schedule, and that’s why it’s a second line medicine rather than the frontline medicine,” says French.
To change this, French believes that patient advocacy is vital, saying that industry and regulatory improvements must be patient-focused, and that there are already decades-old models to follow such as those in the US and the Netherlands.
“The UK has chosen its own, very restrictive approach, which leaves patients marginalized. Cannabis has enormous potential as a medicine, but barriers around education, affordability, quality, and regulation limit its use,” says French.
“If we address these systematically, we can expand access, improve quality, and integrate cannabis into standard medical practice.”
Barnes suggests that there may be a lingering fear around drug policy for political parties, but urges that the matter has nothing to do with recreational use, “this is medicine.”.
“If we keep educating doctors, supporting patients, and collecting robust evidence, I genuinely believe that within the next five years, we’ll see medical cannabis routinely prescribed within the NHS,” says Barnes.
“The science supports it, the patients need it, and the world is moving in that direction.”
While it is clear that medical cannabis has come a long way since its legalization in 2018, these remaining barriers highlight the difficulty patients face when accessing medical cannabis and the hurdles that have yet to be overcome before equitable access is achieved.