What Happens When ADHD and Anxiety Mix Together? And How to Manage Both?

ADHD and anxiety often go hand in hand, but why? This explainer breaks down the complex interplay between attention, arousal, worry, and executive function — and what it means for treatment.
It’s not unusual for people with ADHD to live with anxiety — in fact, up to 50% of individuals with ADHD experience an anxiety disorder at some point. But despite how common this overlap is, the relationship between these two conditions is anything but simple. Understanding how ADHD and anxiety intersect helps patients make sense of what they’re feeling.
What are ADHD and Anxiety — and Why They Overlap
Attention Deficit Hyperactivity Disorder (ADHD) and anxiety disorders are among the most commonly diagnosed mental health conditions, and they frequently co-occur. About 2.5% of adults in the general population have ADHD, and common comorbid conditions include substance use disorders, personality disorders, and mood and anxiety disorders.
Because symptoms of ADHD and its comorbid disorders often overlap, distinguishing between them can be challenging. While ADHD is rooted in executive dysfunction — affecting planning, focus, impulse control, and regulation — anxiety is characterized by chronic worry, heightened arousal, and avoidance behaviors. On the surface, they can look similar: restlessness, distraction, trouble concentrating, irritability.
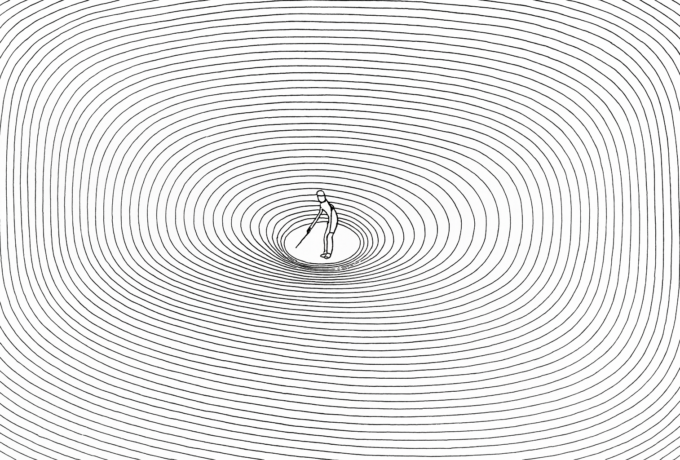
This symptom overlap often causes confusion. A child who zones out in class or fidgets constantly may be misdiagnosed with ADHD when they’re actually anxious — or vice versa. But when the two truly coexist, they can compound each other. For instance, a person with ADHD might forget an appointment or miss a deadline, triggering anxiety about failure or judgment. That anxiety, in turn, makes it harder to focus, creating a vicious cycle.
Clinical guidelines recommend that when ADHD co-occurs with other psychiatric conditions in adults, treatment should typically focus first on the condition causing the greatest impairment.
What ADHD and Anxiety Feel Like
Living with ADHD can feel like trying to follow six conversations at once while forgetting what you were just about to say. Your mind jumps lanes without warning — from a grocery list to a childhood memory to a sudden sense that you’ve forgotten something urgent. Focus is elusive, and time slips through your fingers. Even simple tasks can feel mountainous when your attention refuses to cooperate.
Now add anxiety to the mix. It’s not just restlessness; it’s a constant hum of dread beneath your thoughts, as if something bad is about to happen — even when everything is fine. Your body tenses without permission, your breath shortens, and your mind loops over worst-case scenarios like a broken record. You might procrastinate out of fear, then spiral into guilt or panic because the deadline is now even closer.
Together, ADHD and anxiety can create a uniquely exhausting storm. You may struggle to start tasks because of poor focus (ADHD), but also fear starting them because of what might go wrong (anxiety). You’re both overwhelmed and under-engaged. The day becomes a series of internal negotiations between chaos and fear, lurching between too much stimulation and a total mental freeze.
Neuroscience Behind the Tangle
From a neurobiological perspective, ADHD and anxiety involve distinct — yet interacting — brain systems. ADHD is associated with underactivity in the prefrontal cortex and dysregulation of dopamine and norepinephrine, leading to challenges in maintaining attention and regulating impulses. Anxiety, meanwhile, often involves hyperactivation of the amygdala and related fear circuitry, as well as dysfunction in the body’s stress response system.
Meanwhile, many people with ADHD experience what’s called emotional dysregulation — difficulty managing frustration, stress, and mood swings. This may amplify sensitivity to anxiety triggers. Research shows that anxiety symptoms can make ADHD symptoms worse, while difficulties with executive functions in ADHD, like planning and controlling impulses, can also increase feelings of anxiety. Genetic factors may also play a role. Both ADHD and anxiety have moderate or high heritability (77-88% for ADHD and approximately 30% for anxiety), and certain polymorphisms in dopamine and serotonin genes have been linked to both conditions.
ADHD can also lead to overcompensation with perfectionism — in response to past mistakes or feelings of inferiority. For others, it becomes a form of self-punishment or a way to procrastinate. And when perfectionists fall short of their own or others’ expectations, anxiety and shame often follow.
Why It’s Easy to Miss or Mislabel
ADHD and anxiety often mask or mimic each other, making diagnosis tricky — especially in adults. For instance, ADHD and anxiety both involve inattention, but for different reasons: in anxiety, it’s driven by worry and rumination; in ADHD, it stems from distractibility and a tendency to seek out new or stimulating experiences. Someone with ADHD might appear anxious because they’re constantly behind on tasks, forgetting things, or overwhelmed by unstructured environments. On the flip side, chronic anxiety can cause restlessness, racing thoughts, and difficulty concentrating — all symptoms that look a lot like ADHD.
Clinicians sometimes misattribute ADHD symptoms to anxiety alone, especially if the person is high-functioning or excels in some areas of life. Gender can further obscure the picture: girls and women are more likely to present internalized symptoms (like inattentiveness or anxiety) rather than the stereotypical hyperactivity seen in boys. What’s more, many adults with ADHD grew up undiagnosed and learned to cope through overcompensation, which may mask core symptoms — until life stressors outpace those coping skills.
Without a nuanced evaluation, one condition may be diagnosed while the other goes unnoticed, leading to incomplete treatment. Understanding the overlap and interplay is crucial — not just for accuracy, but for tailoring the right therapeutic approach.
How It Is Treated
Managing ADHD and anxiety together requires a nuanced approach. Stimulants (like methylphenidate or amphetamines) are effective for ADHD and may also reduce anxiety indirectly by improving focus and reducing daily overwhelm. However, in some people, they can intensify anxious symptoms like insomnia. On the other hand, some antidepressants, though not officially approved for ADHD, may help improve both attention and mood.
What usually works best is a combination of approaches:
- Medication is often required. Some clinicians begin by targeting the condition causing the most impairment — for example, stabilizing anxiety to improve sleep and reduce avoidance, or improving attention to reduce chaos and downstream stress.
- Therapy also plays a crucial role. Cognitive Behavioral Therapy (CBT), especially when adapted for ADHD, can help manage distorted thinking and build coping strategies. Mindfulness-Based Cognitive Therapy (MBCT) is another powerful tool, training the brain to stay present and reduce both mental reactivity and impulsivity.
- ADHD coaching or practical skills-based support, like time management systems and external accountability, can dramatically improve daily functioning and reduce anxiety caused by missed tasks or disorganization.
- Lifestyle matters a lot, too. Regular sleep and nutrition, mindfulness-based practices and movement all help regulate both attention and mood. Digital calendars, visual reminders, and structured routines reduce the cognitive load, and calm the mental noise.
Ultimately, treatment works best when both conditions are recognized — and when shame or misunderstanding about one doesn’t get in the way of addressing the other.
Why Recognizing the Overlap Matters
When anxiety is mistaken for ADHD, or ADHD is masked by anxiety, people can go years without appropriate support. This delay can lead to academic struggles, strained relationships, burnout, and low self-esteem. But when the two are seen as interconnected patterns, it becomes easier to identify what’s happening and intervene more effectively.
Families, teachers, and therapists all benefit from understanding this connection. It opens the door to more compassionate, individualized care, and to strategies that help people build a more resilient relationship with their own minds.
How to Navigate the Dual Challenge
Living with both ADHD and anxiety can feel like constantly letting yourself down: missing deadlines, overthinking social interactions, forgetting things that matter. But this dual experience is not a personal failure; it’s the result of two neurobiological patterns that push against each other in exhausting ways.
Navigating this reality means rewriting the story you tell yourself. Instead of “I’m lazy” or “I’m too much,” it’s: My brain works differently — and it’s valid to need support. Self-compassion becomes a daily practice, not a luxury. That might mean using tools like therapy, medication, body-based practices, or ADHD coaching, but also recognizing your wins, however small, and forgiving your missteps.
FAQ:
- Why do some people with ADHD feel “lazy” when they’re actually anxious or overwhelmed?
What looks like laziness is often an inability to act. ADHD and anxiety can make it difficult to prioritize or begin tasks, especially when the brain is flooded with worries or self-doubt. This leads to avoidance, not because of a lack of effort, but because of emotional overload and executive dysfunction.
- How do sensory sensitivities in ADHD affect anxiety levels?
Many people with ADHD experience heightened sensitivity to noise, light, or touch. In overstimulating environments, this can trigger or amplify anxiety. Sensory discomfort may go unnoticed or be dismissed, but it often contributes to emotional fatigue and irritability.
- What’s the connection between ADHD, rejection sensitivity, and social anxiety?
Rejection Sensitive Dysphoria (RSD) is common in ADHD. It’s an intense emotional response to perceived criticism or exclusion, even when minor. This hypersensitivity can lead to avoidance, social withdrawal, or people-pleasing—behaviors that closely resemble social anxiety.
- Can untreated ADHD increase the risk of developing an anxiety disorder later in life?
Yes. When ADHD goes undiagnosed or unsupported, repeated failures, shame, or social struggles can lead to chronic stress and eventually an anxiety disorder. Early support and accurate diagnosis can help reduce this risk.
- How do ADHD and anxiety affect sleep — and how does poor sleep make both worse?
Both conditions can make it hard to fall or stay asleep. Racing thoughts (anxiety) and late-night hyperfocus (ADHD) often collide. Poor sleep then worsens attention, emotion regulation, and stress resilience, creating a self-perpetuating cycle.
- Is it harder to regulate emotions with both ADHD and anxiety?
Yes. Emotional regulation depends on executive function—something already compromised in ADHD. When anxiety is also present, the emotional “volume” is turned up even higher, leading to stronger reactions and longer recovery time after distress.
- How does ADHD-related time blindness contribute to anxiety?
Time blindness makes it hard to estimate how long things take, plan ahead, or feel the urgency of deadlines until it’s too late. This often leads to last-minute scrambling and a near-constant feeling of being behind, which fuels anxiety.
- What should I know about ADHD and anxiety in high-achieving people?
Success doesn’t cancel out ADHD or anxiety. In fact, many high performers rely on coping strategies like overworking or perfectionism to compensate. The pressure to keep up the facade can be exhausting—and it often masks how much they’re struggling internally.