Brain Fog: The Cloud That Hangs Over Our Minds

Search “brain fog” on TikTok and you’ll find videos with millions of views: creators describing days where even simple tasks feel like trudging through quicksand. It’s a phrase that’s gone mainstream in the age of long COVID, burnout, and chronic migraines. But is brain fog just a meme, or a measurable phenomenon?
A 2024 study published in Frontiers in Human Neuroscience offers the most precise map yet of this elusive state of mind. Drawing on data from over 25,000 individuals, researchers identified four dimensions of brain fog: demographics, daily impairments, comorbidities, and cognitive performance.
The results give weight to what many already know intuitively: brain fog isn’t just “in your head.” It’s a real syndrome that carries measurable consequences.
What Is Brain Fog?
Brain fog is defined as a temporary negative shift in cognitive function, often triggered by factors such as illness, hormonal changes, or medical treatments like chemotherapy. The term describes those stretches of time when the mind feels slower, heavier, or oddly out of sync with the world.
Tasks that once felt effortless suddenly feel draining. People describe struggling to pay attention, needing more time to understand speech, or finding simple decisions overwhelming. Others notice gaps in memory, trouble planning, or a frustrating inability to multitask.
Unlike depression, ADHD, or dementia, brain fog is not a recognised mental disorder; it’s a way of naming a state of mind or a cluster of symptoms. Calling it “fog” captures that feeling well. It’s not a permanent storm, but a passing weather system in the mind. With time, support, and care, the haze can lift, and clear thinking often returns.
What Brain Fog Feels Like
Forget the stereotype of absentmindedness. Brain fog is more than forgetting where you put your keys. In the study, people with brain fog were:
- Three times more likely to struggle with focusing or concentrating.
- Twice as likely to lose track of conversations or miss appointments.
- Frequently reporting irritability, poor relaxation, and difficulty with everyday tasks like paperwork or even basic math.
These aren’t minor inconveniences. They’re functional breakdowns that ripple across work, relationships, and self-worth. Imagine trying to file taxes, follow a group discussion, or drive in traffic when your brain refuses to cooperate. For many, that’s a daily reality.
What makes the experience challenging is less the severity of the symptoms than the mismatch they create: you know what you’re capable of, but your brain isn’t meeting you there.
Who’s Most Affected?
The research found a few striking patterns:
- Brain fog was more prevalent among females and slightly older individuals, with an average age of around 36.
- It was strongly tied to long COVID, with sufferers almost 4 times as likely to report foggy cognition.
- Migraines and concussions also stood out as major contributors.
In other words, brain fog isn’t random — it clusters around specific health conditions. And while lifestyle factors, such as poor sleep or fast food intake, showed smaller correlations, they still have an impact.
A Pandemic Spotlight
COVID-19 didn’t invent brain fog, but it turned a fringe complaint into a global headline. Millions who never thought of themselves as “foggy” suddenly found themselves unable to focus acutely during symptoms, which could linger for weeks or months after infection. Research shows that long COVID magnifies the core symptoms of brain fog and that those people with both long COVID and brain fog were 5 times more likely to struggle with concentration.
It makes brain fog a cultural phenomenon as much as a medical one. Entire communities of COVID-19 long hauliers formed online around the shared language of “cloudy thinking,” reshaping how society talks about cognition and fatigue.
Scrolling Through the Fog
For many Gen Z and millennials, brain fog isn’t an occasional lapse — it’s a cultural condition. Ask around and you’ll hear people describing how I can’t focus, I can’t switch off, I’m tired but wired. Social media platforms that once promised connection now blur into endless feeds, leaving young people overstimulated, under-rested, and unable to think straight. “I don’t know anyone my age who hasn’t felt brain fog,” says 25-year-old illustrator Anjali Raj. Her words echo across dorm rooms, co-working spaces, and late-night doom-scrolls.
Social media acts as both a catalyst and a contributor to this issue. It spreads awareness of brain fog while at the same time fueling it, dragging users into loops of reels, quick-fix hacks, and ambient anxiety. As 21-year-old psychology student Esha puts it: “Scrolling has become default.” For her, mindfulness breaks and reading printed books are lifelines, but breaking the cycle feels like swimming against the current.
Experts attribute sleep loss, binge-watching TV shows, and poor gut health as potential underlying contributors. The brain’s glymphatic system — the night shift that clears waste products generated by brain cells — can’t function on four or five hours of restless sleep. Stress eats at focus; anxiety fogs memory. The paradox is sharp: the very generation most fluent in wellness language is also the most trapped in habits that fray attention.

The Science of the Slowed Mind
One of the most interesting findings is that people with brain fog performed slightly worse on cognitive tests — roughly the equivalent of a small but measurable drop in performance. This difference was most evident on the Stroop test, which measures mental flexibility and the ability to filter distractions.
That sounds small, but in real life, it maps onto the exact things people complain about: struggling to block out irrelevant information, bouncing between thoughts without landing, or failing to switch gears when life demands it.
It’s not that brain fog sufferers can’t remember things at all — their memory scores weren’t significantly worse. The issue appears to stem from difficulty filtering distractions, where an excessive number of signals compete for attention, making it more challenging to focus.
Not Just Neurological
Here’s where things get complicated: brain fog isn’t purely a brain issue. The study found substantial overlap with migraine disability scores, anxiety, depression, and poor sleep. It makes brain fog a kind of crossroads syndrome — sitting at the intersection of neurology, psychology, and lifestyle.
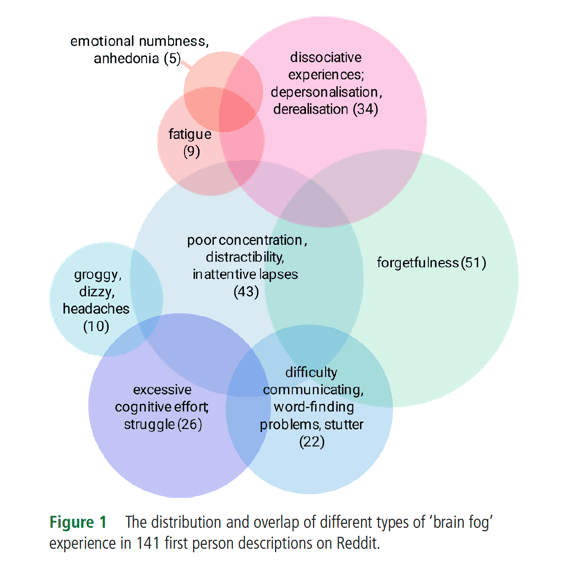
That overlap also explains why people experience brain fog in different ways. Some report it as heavy fatigue, while others describe it as a buzzing static, and still others experience emotional numbness. But the common denominator is the sense that one’s mental sharpness has dulled, often with no clear explanation.
Can You Treat Brain Fog?
In most cases, brain fog fades as the body recovers. Rest, better sleep, supportive environments, and gentle cognitive strategies all play a role in regaining clarity. Research suggests a few starting points:
- Check for comorbidities. If migraines, concussion history, or long COVID are in the picture, brain fog may be a symptom of those underlying issues.
- Address mental health. Anxiety and depression were strongly linked to foggy cognition — managing those could lighten the load.
- Lifestyle tweaks matter. Better sleep, reduced fast food, and more consistent exercise all showed modest associations with clearer thinking.
The key takeaway? Brain fog is rarely an isolated condition. Tackling it means looking at the whole person — physical health, mental health, and environment.
Why This Matters Now
The timing of this research is no accident. In an economy that demands constant focus and productivity, a quarter of adults reporting brain fog (28% in this study) is more than a medical curiosity — it’s a public health and cultural issue.
Brain fog affects not just individuals but also workplaces, schools, and families. It blurs the line between “functional” and “disabled,” often in ways invisible to others. That invisibility can lead to stigma: people are told to “just push through,” even when the science shows measurable impairments.
Researchers argue that brain fog should be evaluated alongside migraine, concussion, and post-viral conditions — not brushed off as a vague complaint. And with machine learning models predicting brain fog with up to 74% accuracy, there’s potential for digital health tools to detect and track it early.
But numbers only tell part of the story. For many, brain fog is about the lived experience of losing a sense of self, being unable to do things that once came naturally. Future research will need to honour that subjective reports matter as much as the cognitive scores. In a culture obsessed with optimisation, brain fog reminds us that the mind is not a machine. Sometimes it slows, sometimes it clouds. The task ahead isn’t just to measure the fog, but to learn how to move with it — and, when possible, clear the air.
FAQ
- Is brain fog the same as ADHD or depression?
Not exactly. ADHD and depression are clinical diagnoses with established criteria, while brain fog is more of a descriptive term for temporary mental sluggishness. That said, the conditions can overlap — many people with ADHD or depression also report foggy thinking.
- How long does brain fog last?
It varies. For some, it’s a few hours after a poor night’s sleep; for others — especially post-COVID or after a concussion — it can last weeks or even months. Persistent brain fog is a sign to seek medical advice.
- Is brain fog a sign of early dementia?
Usually not. Occasional forgetfulness and lack of focus are everyday occurrences in young, otherwise healthy people. However, if the fog is severe, progressive, or significantly impacts daily functioning, a medical evaluation is essential to rule out underlying conditions.
- Can exercise clear brain fog?
Movement boosts blood flow, oxygen, and neurotransmitters linked to focus. Regular activity also improves sleep and reduces stress — two of the primary contributors to mental cloudiness.
- Are there supplements for brain fog?
Some people report benefits from omega-3 fatty acids, B vitamins, magnesium, or adaptogens like ashwagandha. However, supplements aren’t a magic fix; their impact is modest compared to the basics of lifestyle: sleep, nutrition, hydration, and stress management.
- What else can affect brain fog?
Your diet also matters. Research links gut health and inflammation to cognition. Diets high in processed foods and low in fibre may worsen fog as they can increase inflammation, while nutrient-rich, whole foods (such as omega-3s, leafy greens, and fermented foods) may help keep the mind clearer.
- Does caffeine help or hurt brain fog?
Both. A cup of coffee may sharpen focus temporarily, but overuse (or relying on caffeine to replace sleep) can backfire, increasing anxiety and worsening fatigue.