How Autism Spectrum Disorder Rewrites Old Labels

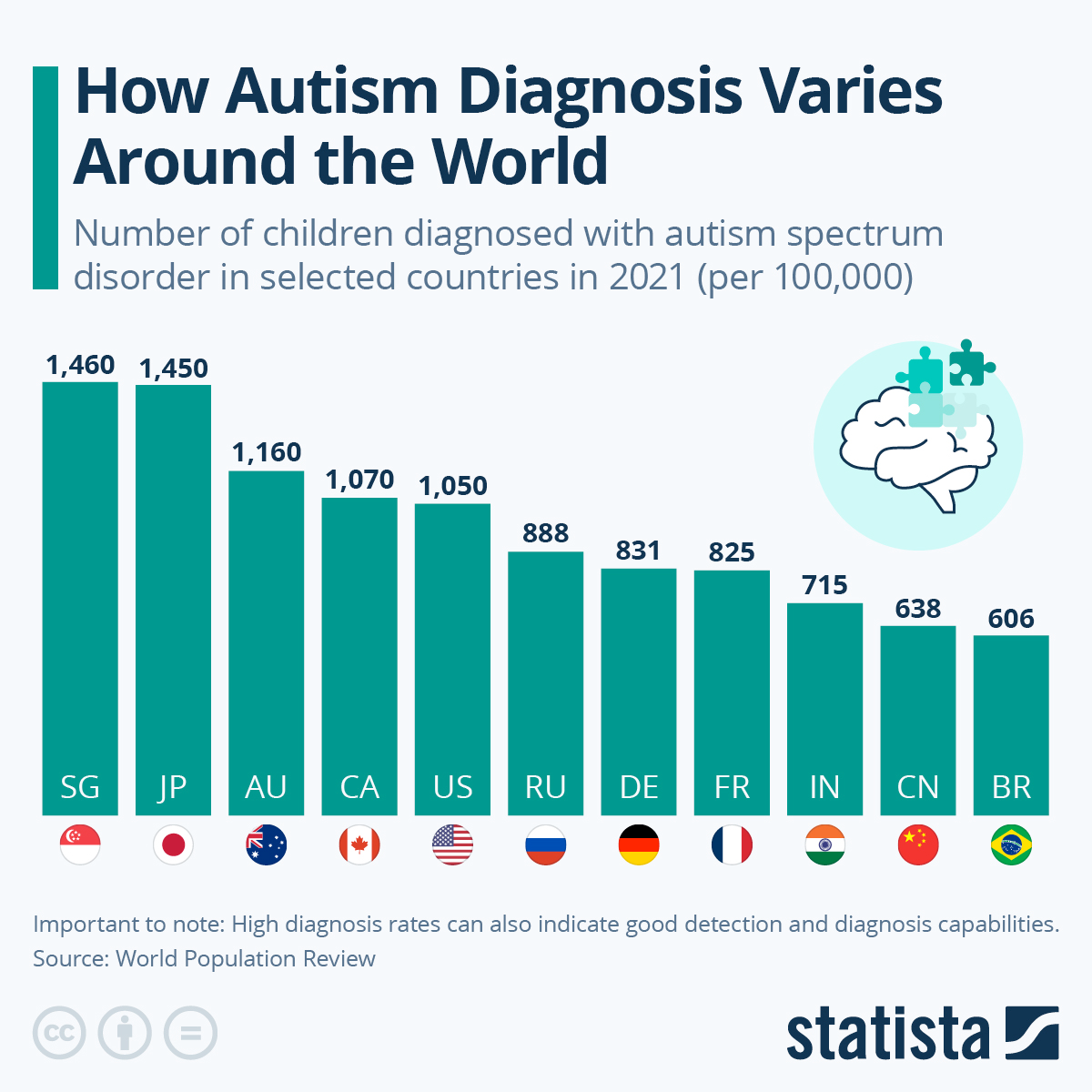
Autism spectrum disorder (ASD) is now seen less as a rigid medical category and more as a spectrum of human diversity. Old terms like Asperger’s syndrome or “high-functioning autism” have been retired, giving way to an approach that values differences instead of ranking them. Globally, approximately 1 in 100 children is estimated to be on the spectrum — a reminder that millions of people worldwide are better understood today through the lens of neurodiversity, where the goal is not to erase differences but to support them.
What Is Autism Spectrum Disorder?
Autism spectrum disorder (ASD) is a lifelong neurodevelopmental condition that changes the way people communicate, behave, and experience the world. Instead of a single disorder, autism is now understood as a spectrum — because traits, challenges, and strengths vary widely across individuals.
Core traits and symptoms
The diagnostic classification DSM-5 defines ASD by two core domains:
- Social communication differences: difficulties with conversation, interpreting body language, or forming relationships. For example, some children may not point to share interest, or may speak in a flat or sing-song voice.
- Restricted and repetitive behaviours: hand-flapping, rocking, repeating phrases, or being intensely focused on specific topics, such as train schedules or video games.
Sensory differences are also common. Some individuals with autism are highly sensitive to bright lights, loud noises, or scratchy clothing, while others seek sensory input by spinning or touching certain textures..
Age of onset and life course
Signs of autism usually begin in early childhood — sometimes as early as 12–18 months. For instance, retrospective video studies have shown differences in gaze and social interest in infants under 1 year. Still, diagnosis often comes later: many adolescents are identified when social demands at school increase, and many adults — especially women — only receive a diagnosis after years of “masking” their difficulties. Masking can include copying peers’ gestures or rehearsing small talk to hide autistic traits.
How The Spectrum System Works
Modern diagnosis doesn’t divide autism into separate categories. Since 2013, the new mental health classification DSM-5 has consolidated all previous subtypes under the umbrella of ASD, as studies have shown that the old conditions overlapped too much to be distinguished. Instead of multiple labels, doctors now describe each person’s place on the spectrum using specifiers that reflect their individual differences.
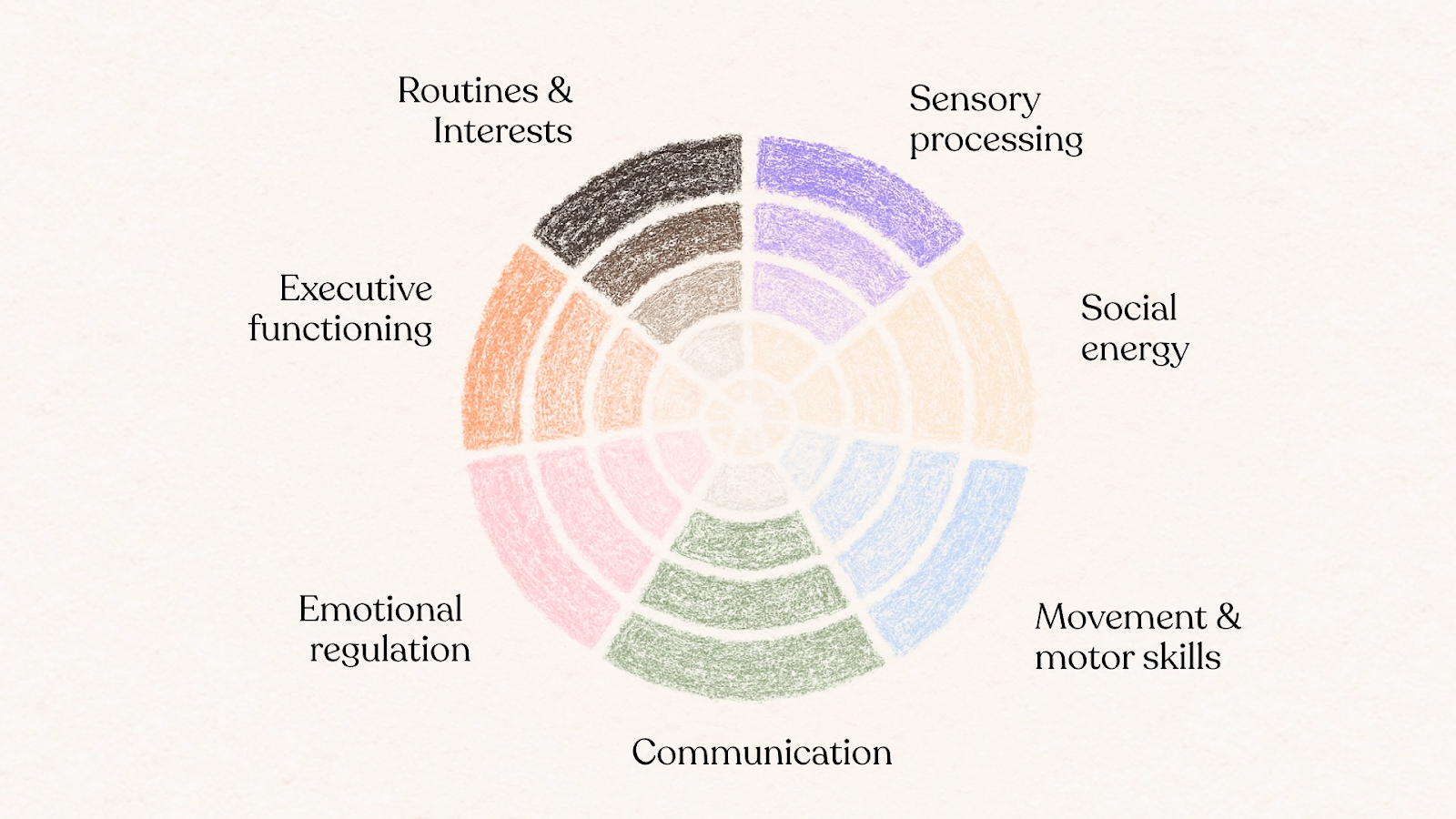
This approach shifts the focus from rigid categories to profiles across key areas of life, such as communication, sensory processing, or motor skills. The mix and intensity of traits can vary significantly from one person to another, which is why two people with the same ASD diagnosis may have completely different strengths and challenges.
To guide support, clinicians also assign levels of need (1–3). These range from requiring minimal assistance to very substantial daily help. The levels are not a measure of intelligence or worth, but a practical way to match services, education, and accommodations to what each person needs to thrive.
Spectrum Conditions Before Reclassification
Before 2013, when the new system was introduced, autism was categorised into separate groups. These subtypes include Asperger’s and other diagnoses — now unified under the broader diagnosis of ASD. Experts described the differences between the conditions as follows:
Classic autism
Previously called “autistic disorder,” this was the most widely recognised form of autism. It often involved apparent difficulties with language, social interaction, and repetitive behaviours beginning in early childhood. Many children in this group required substantial support with communication, learning, and daily living.
Asperger’s syndrome
Added to the diagnostic classification in 1994, Asperger’s syndrome describes individuals with average or above-average intelligence and no language delay, but with difficulties in social reciprocity, sensory processing, and restricted interests. Since 2013, the label has been retired, though many people still identify with it as part of their personal or community identity.
PDD-NOS
Clinicians used pervasive developmental disorder–not otherwise specified when someone showed autistic traits but did not meet the full criteria for another subtype. It became a catch-all diagnosis, which created confusion and inconsistent treatment pathways. Under DSM-5, these individuals are now diagnosed with ASD.
Childhood disintegrative disorder
A rare condition where children typically develop for the first few years of life, then experience a severe loss of skills — including speech, social abilities, and motor coordination. It is now considered part of the autism spectrum but remains an unusual and extreme presentation.
In practice, the recent reclassification means that instead of debating whether someone has classic autism or something else, doctors now focus on describing the person’s profile of traits and co-occurring conditions. The spectrum model captures both commonalities and differences, helping move away from outdated labels like “low” or “high functioning.”
How Autism Is Diagnosed Today
Autism is no longer divided into separate categories or diagnoses. Instead, doctors use the umbrella diagnosis of autism spectrum disorder (ASD), supported by standardised tools and developmental history.
Parents, teachers, or pediatricians are often the first to raise concerns. A common screening tool is the M-CHAT-R/F (example) — a brief questionnaire for children between 16 and 30 months old. It helps flag possible traits and guides referrals for more detailed evaluation.
Besides screenings, psychologists and psychiatrists use structured instruments to confirm a diagnosis:
- ADOS (Autism Diagnostic Observation Schedule) — observes play, communication, and problem-solving.
- ADI-R (Autism Diagnostic Interview–Revised) — parent interview covering development and behaviour.
- CARS (Childhood Autism Rating Scale), SRS (Social Responsiveness Scale), SCQ (Social Communication Questionnaire) — questionnaires and rating scales.
These tools provide a complete picture of strengths, challenges, and daily functioning, rather than a simple yes/no outcome.
ASD can be identified in toddlers, but many people are diagnosed later in adolescence or adulthood — especially women, who may mask traits for years. Early detection is crucial, as intervention in the first years of life is associated with more robust language, social, and adaptive outcomes.
ASD Treatment and Support
Autism spectrum disorder support is not about “fixing” autism but about helping people build on their strengths and manage daily challenges. The most effective plans are individual, since every autistic person has unique abilities and needs.
Early intervention
Starting therapy early helps children develop communication, social, and learning abilities. Common supports include:
- Speech therapy to strengthen language and interaction.
- Occupational therapy to improve daily skills and manage sensory sensitivities.
- Play-based learning to build social and cognitive development.
Behavioural and developmental therapies
Research-backed approaches remain central in autism care:
- Applied Behaviour Analysis (ABA) — structured skill-building.
- Early Start Denver Model (ESDM) — play-based intervention for young children.
- Pivotal Response Treatment (PRT) — naturalistic, motivation-focused therapy.
- TEACCH program — structured teaching with visual supports.
Social and psychological support
Beyond early years, therapy may focus on:
- Social skills groups to practice friendships and teamwork.
- Cognitive-behavioural therapy (CBT) adapted for autistic individuals to manage anxiety.
- Peer mentoring and support networks to reduce isolation and build confidence.
The modern approach emphasises accommodation and acceptance as much as therapy: adapting classrooms, workplaces, and communities so autistic people can thrive.
What is PDA and Why It Deserves Its Own Spotlight
Pathological Demand Avoidance is a profile on the autism spectrum where a person strongly avoids everyday demands — from getting dressed for school to completing simple tasks at work.
This avoidance is not simple defiance; it is often driven by overwhelming anxiety and a need for control. Common symptoms include using distraction or excuses to avoid requests, sudden mood swings when pressured, and a paradoxical mix of surface-level sociability with more profound difficulties in relationships.
Although PDA is often discussed within the autism spectrum, it stands out because of its unique pattern of behaviours and the ongoing debate about its status. Unlike the “historical” merged subtypes, PDA wasn’t previously part of the autism-related classifications. Instead, it emerged from clinical observations in the UK, where psychologist Elizabeth Newson first described it in the 1980s.
Why highlight PDA separately?
- Distinct behavioural profile: PDA traits — such as extreme demand avoidance linked to anxiety, surface sociability, and sudden outbursts under pressure — do not fit neatly into classic autism criteria.
- Practical relevance: Many families and schools find that recognising PDA helps them tailor support strategies, such as reducing direct demands or using collaborative approaches.
Highlighting PDA separately is significant because it demonstrates how the spectrum framework is still evolving. While old categories have been retired, new profiles like PDA continue to challenge the boundaries of how autism is defined, diagnosed, and supported.
Emerging Diagnostics and Therapies
Research into autism spectrum disorder is moving beyond observation toward tools that may allow earlier and more objective detection. Scientists are testing machine learning models trained on genetic data, brain scans, and even gut microbiome profiles to recognise subtle biological markers of autism. Other studies explore eye-tracking in infants, where atypical gaze patterns are detectable within the first year of life, and MRI-based methods that highlight differences in brain connectivity. These approaches are still experimental, but they open the possibility of diagnosis long before traditional behavioural signs appear.
Alongside research in diagnostics, technology is also being used to expand support. Digital platforms and apps help children practice communication and social skills at home, while AI-based systems are being developed to personalise learning plans and guide therapy choices. Although these innovations are not yet standard practice, they reflect a shift toward more precision-based, individualised care for autistic people, combining scientific progress with a neurodiversity-informed approach.
FAQ
- What is the difference between Asperger’s and autism spectrum disorder?
Since 2013, Asperger’s is no longer a separate diagnosis. It is now included under the umbrella of autism spectrum disorder, which better reflects the variety of traits and support needs.
- What are common signs of autism?
Autism symptoms include challenges with social communication, restricted or repetitive behaviours, and sensory differences such as sensitivity to noise or light.
- At what age do signs of autism usually appear?
Early signs can emerge between 12 and 18 months, including a lack of pointing, limited eye contact, or delayed speech development. However, some people are not diagnosed until adolescence or adulthood.
- Can adults be diagnosed with autism?
Yes. Many adults, especially women, discover their autism later in life after years of masking or being misdiagnosed with anxiety or depression.
- What is PDA? Is it part of the autism spectrum?
Pathological Demand Avoidance (PDA) describes extreme avoidance of everyday demands, often driven by anxiety. It is not an official diagnosis in some classifications, but is widely recognised as a profile within the autism spectrum, especially in the UK.
- What treatments are evidence-based for autism?
There is no cure, but therapies such as speech and occupational therapy, ABA, and play-based models (e.g. the Early Start Denver Model) help build skills and promote independence.