Reading Navigation
When Chronic Pain Doesn’t Stop, Could Ketamine Therapy Be the Answer?

About one in five adults in Europe — roughly 150 million people — live with chronic pain lasting more than 6 months. In some countries, the rates may be even higher: moderate-to-severe chronic pain affects nearly 19% of adults1and significantly impacts work, relationships, and mental health. Worldwide, the numbers look similar. Around 20% of adults2suffer from chronic pain, and about 10% are newly diagnosed each year with persistent or worsening cases.
For many, the standard prescription is strong painkillers — typically opioids, such as codeine, oxycodone, and fentanyl. Yet these only work for a fraction of patients, often lose effectiveness, or bring their own problems like dependence and side effects.
That’s where ketamine infusions come in. Once known mainly as an anaesthetic — and, outside medicine, a party drug — ketamine is being re-evaluated as an option for people left behind by traditional treatments. Early studies suggest pain relief, sometimes within hours after a session. But how solid is the evidence, and what risks come with it?
What Is Chronic Pain and Why Is It Hard to Treat?
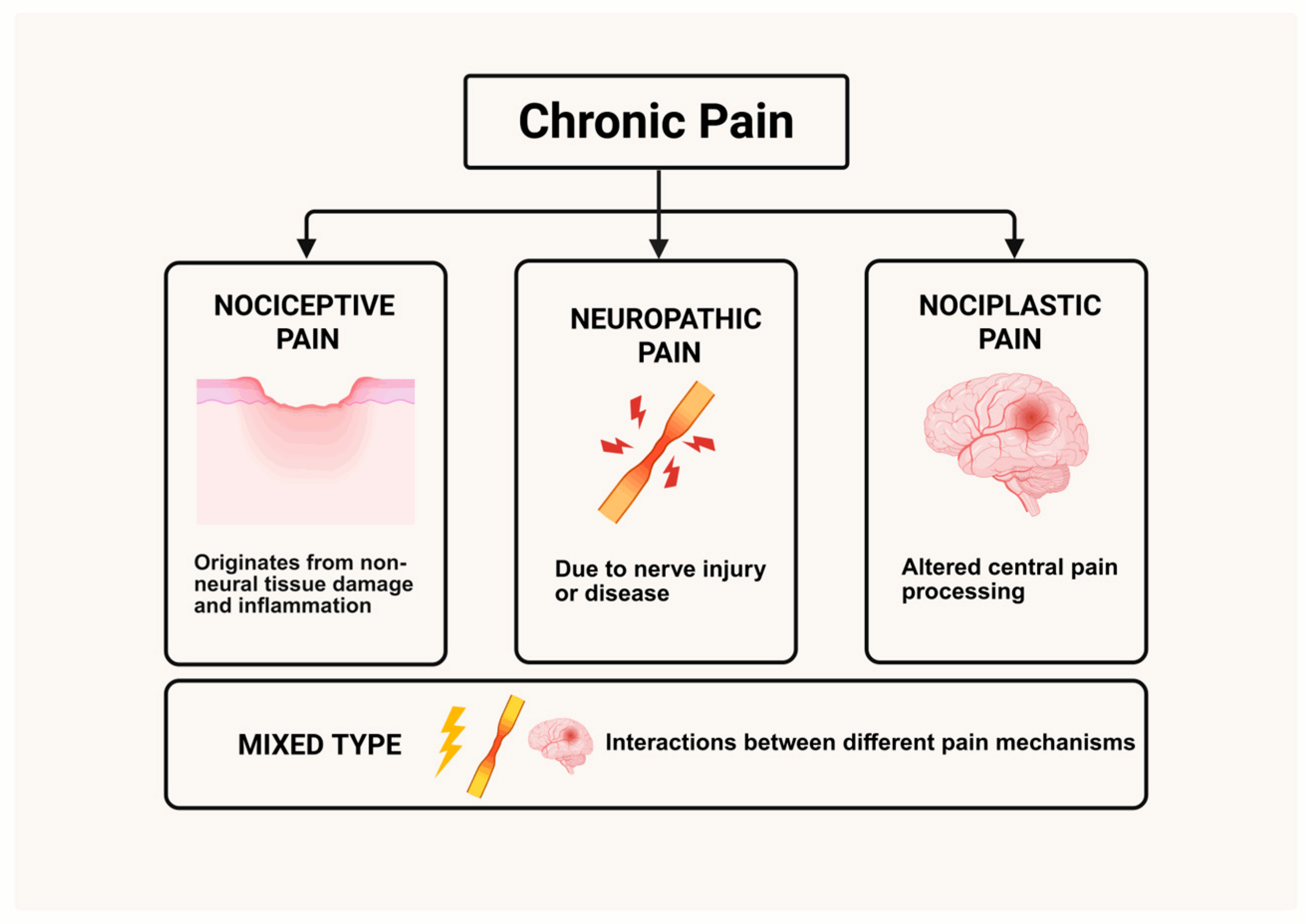
The International Association for the Study of Pain (IASP) defines chronic pain as pain that persists for more than 3 months, extending well beyond the time the body typically requires to heal. Specialists stress that it’s not just a symptom that refuses to go away. Over time, chronic pain can become a condition of its own, rewiring the nervous system and making it overly sensitive. Experts usually describe three main types of chronic pain:
- Neuropathic pain comes from the nerves themselves being damaged or irritated. It’s often described as burning, stabbing, or like an electric shock. Everyday examples include diabetic neuropathy (nerve damage from long-term diabetes), sciatica (pain shooting down the leg from a pinched nerve), or the lingering sting some people feel after shingles.
- Nociceptive pain happens when there’s clear injury or strain on the body. It usually feels like a steady ache, throbbing, or stiffness. Typical examples include osteoarthritis (worn joints that become swollen and painful), sports injuries such as sprains, or the deep back pain that develops over time due to years of heavy lifting or poor posture.
- Nociplastic pain is trickier: here, the nervous system itself is overactive, amplifying pain signals even when doctors can’t find visible damage. It often shows up as widespread or hard-to-pinpoint pain. Conditions like fibromyalgia fit here, and migraine3 is also usually classified as nociplastic, since the brain’s pain pathways become hypersensitive even without a single obvious injury.
The challenge is that common painkillers often don’t do much here. Opioids, anti-inflammatories, anticonvulsants — all together they only bring real relief to about 30–40% of patients4. Opioids especially lose power as tolerance builds, and extended use can spiral into dependence, dangerous side effects, or even a cruel twist called opioid-induced hyperalgesia5— when the medication makes pain worse instead of better.
That leaves millions of people stuck: daily life is shaped by pain, while the strongest painkillers in the cabinet either don’t work well enough or open the door to even bigger problems.
Ketamine Could Break the Chronic Pain Cycle
Most painkillers work in a narrow way6: they either dull nerve endings, calm inflammation, or block pain signals as they travel to the brain. It can help with short-term pain, but chronic pain is different. Over time, the nervous system itself changes, becoming hypersensitive — a state known as central sensitisation. That’s why traditional strong painkillers often fail. They mask the symptoms for a while but rarely touch4 the deeper rewiring that drives chronic pain.
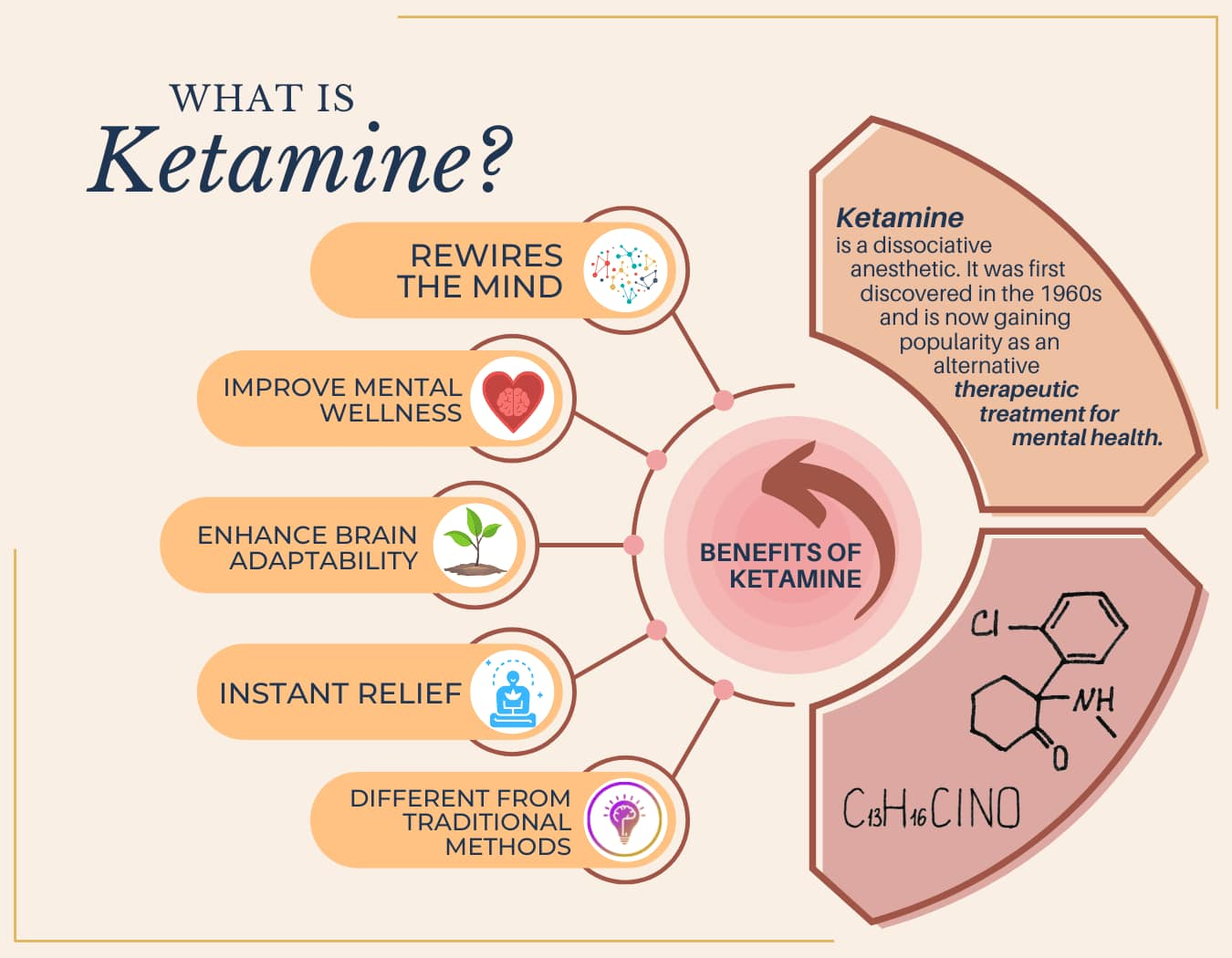
Ketamine is different. Best known as an anaesthetic, today it’s also being studied as a therapy for chronic pain and treatment-resistant depression.
By blocking NMDA receptors — the brain’s “amplifiers” for pain — it can interrupt7 the wind-up process that makes signals feel louder and more unbearable. Clinical studies show8 that even in patients with treatment-resistant conditions like complex pain syndrome or long-term back pain, low-dose infusions can bring meaningful relief when opioids no longer help.
At the same time, ketamine also touches other brain systems, including those linked to opioids (pain relief), serotonin and dopamine (mood), and GABA (calm and relaxation). That’s why many patients report8 not only less pain but also improved sleep, a lighter mood, and an overall better quality of life.
What makes ketamine especially interesting is its dual action. Beyond dampening pain signals, it can also lift mood, reduce anxiety, and improve sleep. In fact, research shows that patients with both chronic pain and depression often respond best. It matters because pain and mood feed each other: when one improves, the other usually follows. This effect makes ketamine a unique candidate in the search for alternatives “beyond painkillers.”
Key Scientific Facts on Ketamine for Chronic Pain
- −41% pain reduction: In a 2023 clinical study8 of 73 patients on long-term oral ketamine, pain scores dropped by nearly half.
- +62% improvement in quality of life: The same study reported a significant improvement in sleep, daily activity, and overall well-being.
- Up to 8 weeks of relief: Meta-analyses show9 that a single ketamine infusion can ease pain for as long as 2 months, although the effect typically fades by 12 weeks. Longer or repeated infusions tend to bring stronger, though not universal, benefits.
- Around 1 in 3 patients report8 no side effects, while others note temporary dizziness, nausea, or vivid dreams. Serious complications remain rare in medical use but require monitoring.
- 329 patients, 1 year, 2 diagnoses: A French cohort found that people with both chronic pain and depression were most likely to benefit, with some maintaining relief for a year. The proportion of reduction of pain mediated by depression was 64%.
- 19% of adults in Europe report moderate to severe chronic pain — yet standard painkillers are effective in only 30–40% of patients9. This gap explains why studies explore ketamine for pain management.
Taken together, these findings show ketamine is not a miracle cure — but for some patients trapped in the cycle of chronic pain, it can bring meaningful and lasting relief.
Ketamine Infusion Therapy: How Does It Work?
In pain clinics, ketamine is given in low doses through an intravenous infusion. Patients sit or lie down while the substance drips slowly into the bloodstream over several hours. The amount is significantly smaller than what’s used in surgery, and doctors monitor heart rate, blood pressure, and oxygen levels. Sometimes extra medicines like benzodiazepines or clonidine are added10 to reduce side effects such as restlessness or vivid dreams.
During the session, ketamine infusions calm down the brain’s “pain amplifiers” while also bringing calm — a double effect that makes them very different from traditional “numbing” painkillers.
Not everyone with chronic pain is offered this therapy. Ketamine infusions are usually considered for patients whose pain has not improved with standard treatments such as opioids or anti-inflammatories. Before starting, most clinics require11 a complete medical evaluation, including medical history, current medications, and screening for conditions like heart disease, liver problems, or psychiatric disorders. If a patient is eligible, the therapist sets up a treatment plan, which may start8 with a short trial infusion to assess the body’s response before scheduling a full course.
The New Era of Chronic Pain Management
The future of ketamine therapy lies in making it easier, safer, and more targeted. Today, most patients receive intravenous infusions; however, researchers are testing nasal sprays, oral tablets, and sublingual lozenges that could bring relief without the need for a hospital setting. Intranasal esketamine, already approved for depression under the brand name Spravato, is one of the most promising candidates.
Another key step is personalisation. As patients with both chronic pain and depression often respond best, future protocols may include screening tools to identify who benefits most. In contrast, large patient registries could help7 standardise safe dosing and reduce risks.
Still, ketamine is not the only hope on the horizon. Researchers are also studying psychedelic-assisted therapy (psilocybin, MDMA), neuromodulation techniques like transcranial magnetic stimulation, and mind-body approaches that combine medication with physiotherapy. Together, these efforts point toward a future where chronic pain is managed not just with stronger drugs, but with more holistic and innovative care.
FAQ
- What is ketamine infusion therapy?
It’s a medical procedure where low doses of ketamine are delivered into the bloodstream through an IV drip. Unlike recreational use, it happens under medical supervision. The goal is to “reset” how the nervous system processes pain.
- How is ketamine different from traditional strong painkillers?
Unlike opioids or anti-inflammatories, ketamine doesn’t just numb pain. It works on NMDA receptors in the brain to calm down “pain amplifiers” and can also improve mood and sleep.
- Is ketamine infusion therapy safe?
Most patients tolerate it well. About 1 in 3 reports no side effects at all. The most common ones are dizziness, nausea, or vivid dreams — usually temporary. Serious risks are rare under medical supervision.
- What types of chronic pain respond best to ketamine infusions?
Studies show promising results for neuropathic pain (like nerve damage or post-shingles pain), complex regional pain syndrome, and some forms of chronic back pain. Patients with both pain and depression may benefit the most.
- What are the effects of ketamine beyond pain relief?
Besides easing pain, ketamine can lift mood, reduce anxiety, and improve sleep quality — making it different from traditional painkillers that only target physical symptoms.
- What other treatments exist for chronic pain?
Options include physiotherapy, psychotherapy, neuromodulation techniques, and even emerging approaches like psychedelic-assisted therapy. Often, the best results are achieved by combining several methods.