OCD Explained: A Complete Guide to Obsessive-Compulsive Disorder

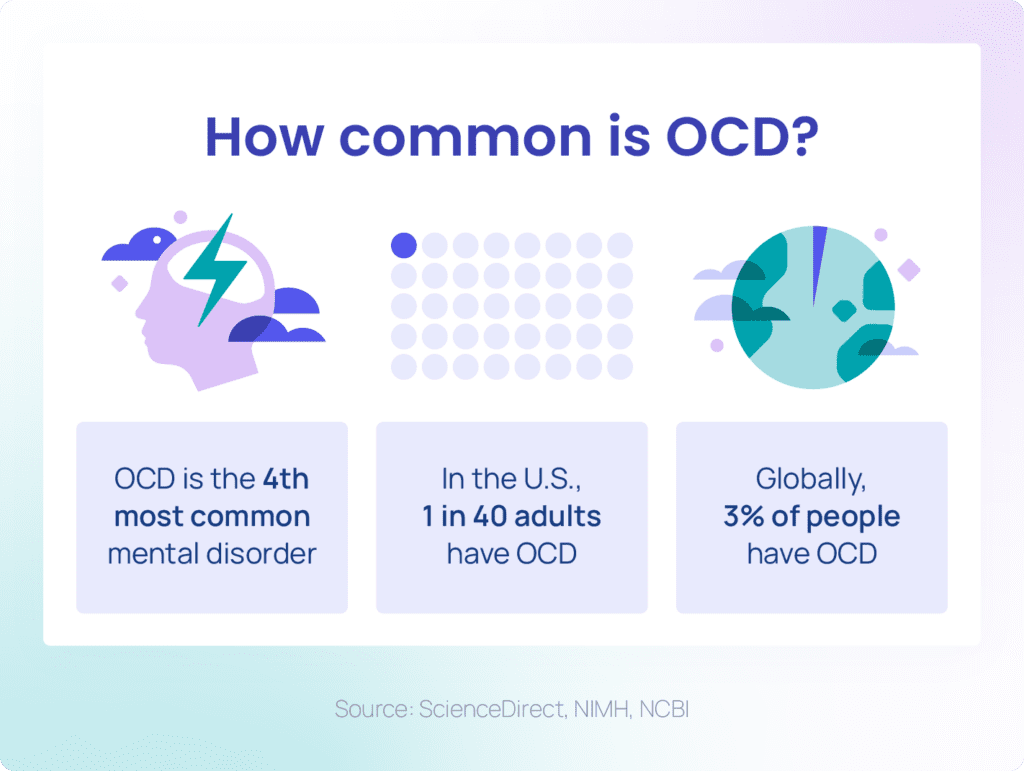
OCD, or obsessive-compulsive disorder, is more common than we used to think — 2–3% of the people in the world experience it at some point in their lives. Around 1.2% meet the criteria in any given year, according to Pathlight Mood & Anxiety Center — that means millions worldwide live with the disorder. Obsessions, compulsive behaviors, and intrusive thoughts are not simply habits or preferences. They are attempts to ease distress or prevent a feared outcome. How else does OCD affect daily life?
What Is Obsessive Compulsive Disorder (OCD)?
Obsessive-compulsive disorder is a mental health condition that causes unwanted, intrusive thoughts (obsessions) and repetitive actions or mental rituals (compulsions). According to the Diagnostic and Statistical Manual, OCD symptoms must take up a significant amount of time, cause distress, and not be explained by another condition.
The COVID-19 pandemic likely led to an increase in obsessive and compulsive symptoms in young people in 2020. The constant reminders to wash hands and disinfect surfaces often reinforced compulsive cleaning rituals, making daily life even more challenging.
The condition rarely exists in isolation. OCD often overlaps with other mental health issues such as anxiety, depression, or ADHD. This combination can make symptoms harder to recognize and more difficult to treat without professional help. Major depressive disorder (MDD) is the most common co-occurring mental health condition associated with OCD. People with OCD and depression often report more severe symptoms, making daily life even more challenging.
Far from being just a “quirk” or a preference for neatness, OCD is a serious medical condition recognized by institutions like the American Psychiatric Association and the NHS in the UK. Understanding what OCD really is helps reduce stigma and encourages people to seek effective treatment.
OCD Behaviour and Common Symptoms
Not every routine or habit is a sign of obsessive-compulsive disorder. Many people like to double-check that the door is locked or prefer a tidy workspace. With OCD, however, these actions are driven by obsessive thoughts — intrusive worries or images that keep repeating — and compulsions, which are repetitive behaviors done to reduce the distress they cause.
Obsessions are unwanted ideas or fears that feel impossible to control, while compulsions are the rituals or acts someone feels pushed to perform. For a diagnosis, these symptoms must significantly impact daily life and occur frequently each day. This is the key factor that sets it apart from “neatness” or simply “being tidy.”
Some common examples of OCD behaviour in everyday life include:
- Checking — repeatedly making sure appliances are off, doors are locked, or tasks are complete.
- Cleaning — excessive handwashing or scrubbing surfaces to relieve fear of germs or contamination.
Ordering and arranging — feeling that objects must be placed “just right” or in perfect symmetry.
These actions may offer temporary relief, but the cycle of obsession and compulsion quickly returns. This makes OCD much more than just a personal quirk — it can become an exhausting daily struggle without proper support.
How OCD Impacts Daily Life
OCD can appear in many forms. Still, researchers often group obsessions and compulsions into a few well-studied patterns. These go far beyond tidiness or habit:
Fixation on Cleanliness and Fear of Contamination
People with this form of OCD are often haunted by intrusive thoughts like “I might get sick if I touch that doorknob” or “my family could be harmed by germs on these surfaces.” Compulsions may include washing hands dozens of times, showering repeatedly, or disinfecting the same object until the skin becomes sore or the surface wears down. In the UK, a controversial reality show called Obsessive Compulsive Cleaners put this compulsion in the spotlight — following people obsessed with cleanliness as they enter the cluttered homes of hoarders and try to make them tidier.
Double-Checking and Reassurance
Obsessions might involve fears such as “I could burn down the house if I left the stove on” or “maybe I hit someone with my car without realizing it.” Typical compulsions are returning home multiple times to check appliances, rereading emails to ensure no mistake, or asking loved ones again and again for confirmation that nothing bad happened.
Symmetry and Order
Some individuals experience a powerful sense that things must be perfectly balanced or aligned, driven by thoughts like “if these books aren’t even, something bad might happen” or “I can’t relax until the form of the pillow feels exactly right.” Compulsions may include arranging objects into precise patterns, counting steps to make them symmetrical, or repeating an action until it produces the “just right” feeling.
Intrusive Thoughts
OCD can also appear in the mind alone. A person may experience unwanted ideas like “what if I hurt someone I love”, “did I just sin”, or disturbing sexual images. These thoughts do not reflect the person’s values, yet they create intense shame and fear. Compulsions may be invisible: silently repeating prayers, mentally reviewing past actions for reassurance, or avoiding situations that might trigger the thoughts.
Irrational Fears in Children and Adolescents
In young people, obsessions may appear as fears like “if I don’t tap the desk three times, my parents will get hurt” or “I must keep my toys lined up or something bad will happen.” Compulsions often include repeating rituals before bed, avoiding certain numbers, or asking adults for constant reassurance. These behaviors can disrupt schoolwork, friendships, and family routines.
OCD Tests and Diagnostics
There’s no single test that can confirm OCD. Diagnosis usually combines clinical interviews with recognized tools. The most popular include:
- DSM-5 and Interviews
Psychiatrists use the DSM-5 guidelines and ask detailed questions about thoughts, behaviors, and how much they interfere with daily life. - Y-BOCS and OCI
Scales like the Yale-Brown Obsessive Compulsive Scale (Y-BOCS, example) and the Obsessive Compulsive Inventory (OCI, example) help measure the type and severity of symptoms. They are often used to track treatment progress. - Online OCD Tests
Quick OCD tests can raise awareness, but they cannot provide a full diagnosis. Only a qualified professional can confirm OCD and suggest treatment.
OCD vs OCPD (Obsessive Compulsive Personality Disorder)
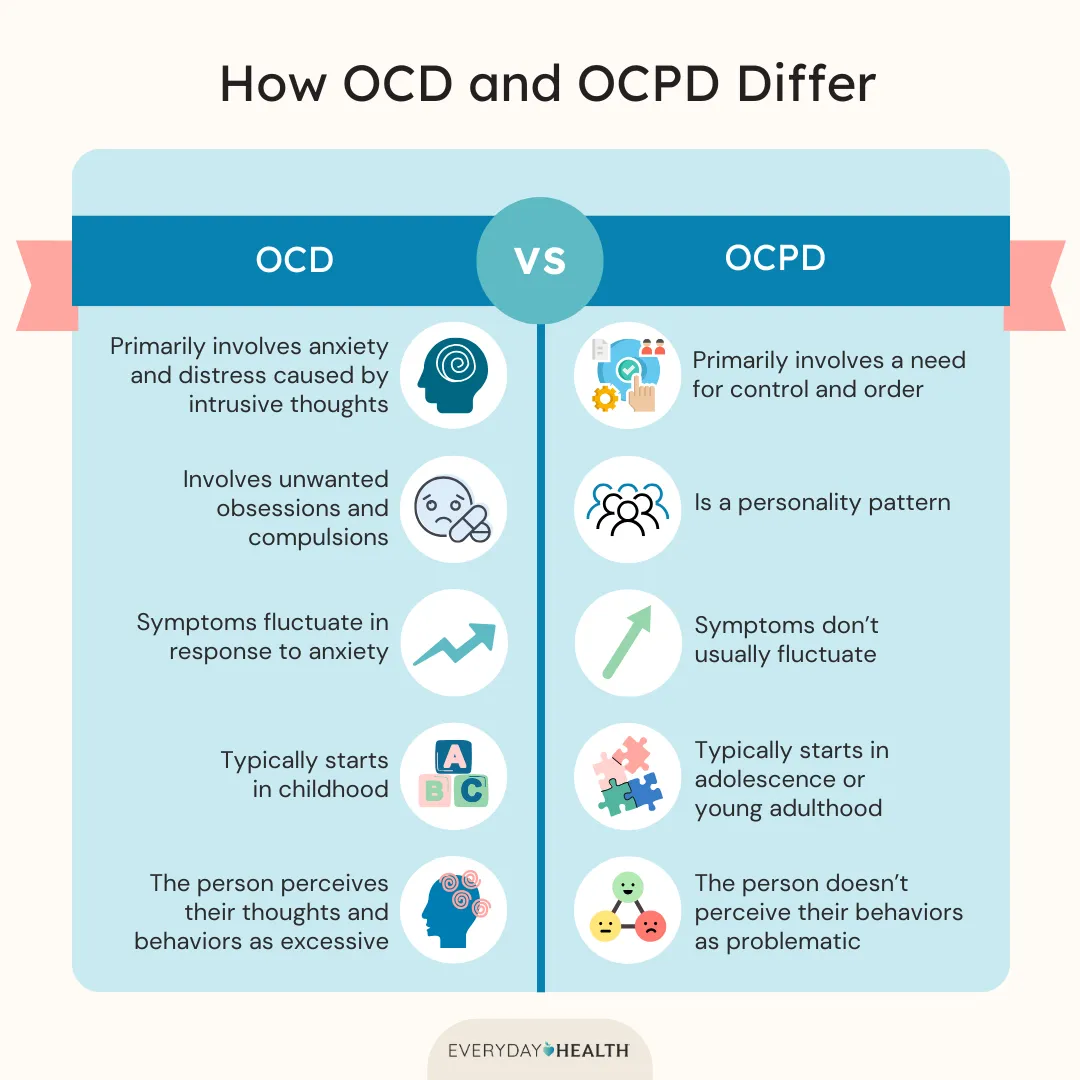
Although the names sound similar, OCD and OCPD are two very different conditions. This confusion often leads people to think they have OCD when they are simply perfectionistic or highly organized.
- Obsessive Compulsive Disorder (OCD) is an anxiety-related condition defined by obsessions and compulsions performed to reduce distress. A person with OCD usually recognizes that their thoughts and actions are excessive, yet feels unable to stop them. For example, someone may wash their hands repeatedly because of a fear of contamination, even when they know the risk is irrational.
- Obsessive Compulsive Personality Disorder (OCPD), in contrast, is a personality disorder. It is about a rigid pattern of thinking and behaving. People with OCPD often place extreme value on control, order, rules, and perfectionism. For example, they may insist that tasks are done “the right way,” have difficulty delegating, or struggle to relax if things are not organized. Unlike OCD, these traits are often seen by the person as logical or even beneficial, not distressing.
The key difference is that OCD causes distress and disrupts life through unwanted thoughts and rituals, while OCPD reflects a consistent personality style of perfectionism and control that feels natural to the person. One is a disorder of anxiety; the other is a personality pattern.
OCD Treatment and Medication
OCD is highly treatable, though it often requires a mix of therapy, medication, and lifestyle support. Research shows that the right treatment can significantly reduce obsessive thoughts and compulsive behaviors, helping people regain control of their lives.
CBT and ERP
The gold standard for OCD treatment is Cognitive Behavioral Therapy (CBT), especially a method called Exposure and Response Prevention (ERP). ERP helps people gradually face their fears while resisting the compulsions. About 75% of adults with OCD see improvement with ERP, and combining it with medication often boosts results.
Medication for OCD
Doctors often prescribe SSRIs (selective serotonin reuptake inhibitors), a class of antidepressants that can reduce OCD symptoms. In some cases, additional medications like quetiapine or aripiprazole may be used when first-line treatments are not enough.
Everyday Habits
Beyond therapy and medication, daily strategies can also help manage OCD. Practices like mindfulness and journaling may reduce stress, while support groups and open conversations with family can lessen feelings of isolation. As Hopkins Medicine notes, treatment is most effective when professional care is paired with strong daily support.
Emerging Therapies for OCD
In recent years, researchers have begun to investigate the potential of psilocybin, the active compound in psychedelic mushrooms, for OCD treatment. Early studies suggest that a single 10 mg dose of psilocybin may reduce compulsive cycles by altering brain connectivity and neural flexibility. While still experimental, these treatments remain promising.
For people who don’t respond to standard treatments, other approaches are being studied. These includetranscranial magnetic stimulation (TMS) and ketamine infusions— shown to provide rapid relief for some patients, though the effect is often short-term.
Breaking The Stigma
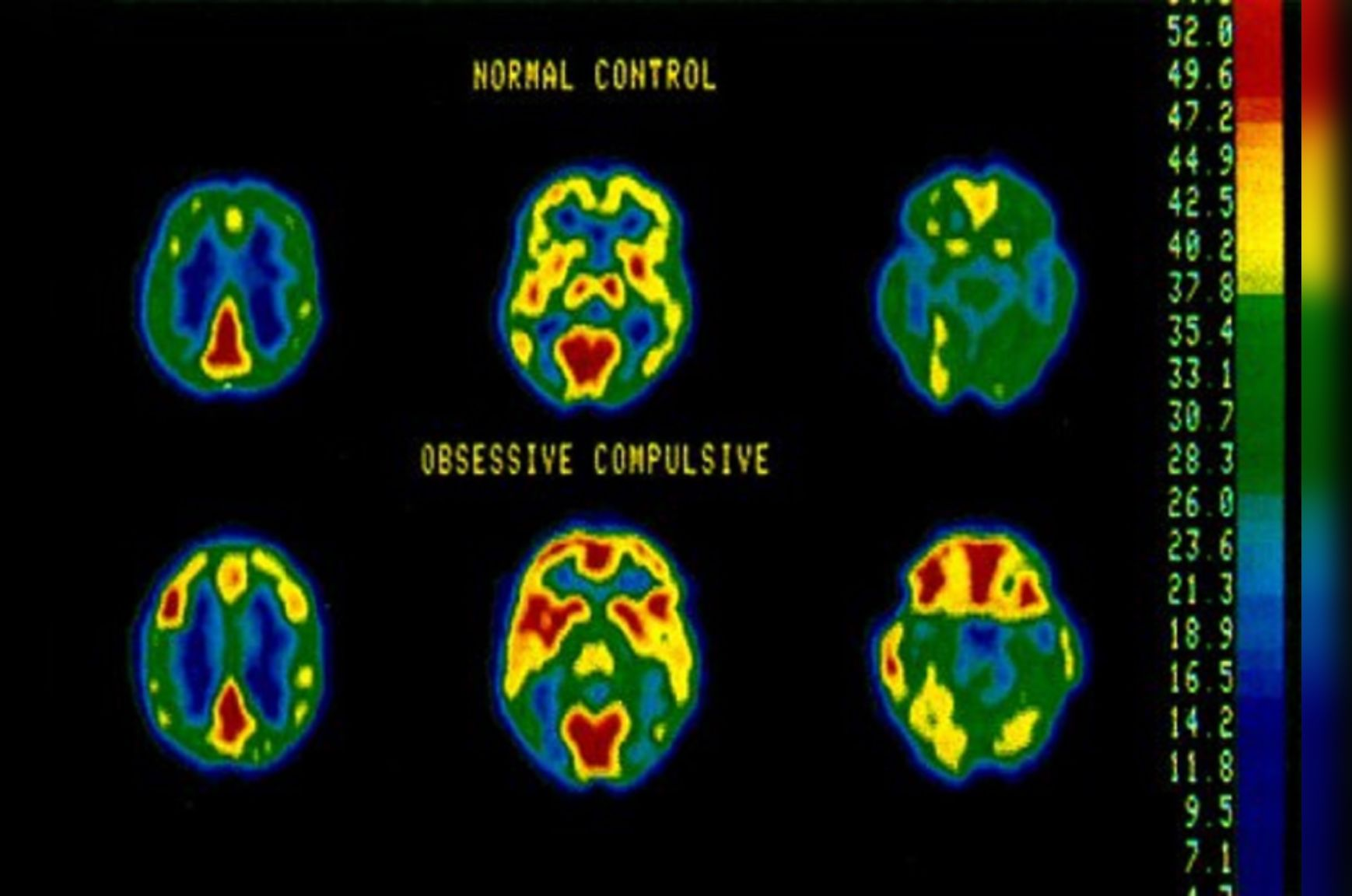
OCD is not a character flaw, a choice, or a result of weak willpower. It’s a legitimate neurobiological condition that affects brain circuits involved in decision-making, habit formation, and anxiety regulation. People with OCD are dealing with a medical condition that responds well to proper treatment.
Recovery from obsessive-compulsive disorder is a journey that requires patience, persistence, and professional guidance. But with today’s evidence-based treatments and growing understanding of the condition, there is genuine hope for everyone affected by OCD. With the right care and prospective therapies, recovery is not just possible — it is within reach.
FAQ:
Can you have OCD without visible compulsions?
Yes. Some compulsions are mental, like silent counting or repeating prayers.
Does OCD usually start in adulthood?
No. It often begins in childhood or teenage years, though adult onset is possible.
Does OCD affect children differently from adults?
Yes. In children, symptoms often mix with tics, anxiety, or attention problems.
Can OCD be treated successfully?
Yes. Cognitive Behavioral Therapy and medications like SSRIs help most people.
Is OCD linked to other disorders?
Yes, OCD often co-occurs with depression, anxiety, or ADHD.
Is OCD somehow genetic?
Yes. Research shows a strong hereditary component, especially in early-onset cases.