How Long Does Ketamine Work for Depression?

*Disclaimer: The information provided in this article is for general educational purposes only and is not intended to diagnose, treat, cure, or prevent any medical condition. Always seek the advice of your physician or another qualified health professional. Do not disregard professional medical advice or delay seeking it because of something you have read here.
Depression is a complex, chronic, and often relapsing condition. It’s more widespread than it may seem at first glance: the WHO reports, around 5,7% of adults suffer from depression, approximately 332 million people in the world. On a spectrum of depressive disorders, treatment-resistant depression (TRD) stands apart. As the name suggests, this type does not respond to standard, first-line therapeutic options for depression: antidepressants (SSRI or SNRI) and psychotherapy. For some patients, these solutions fall short, and unfortunately, this group is not small — up to 30% of individuals with depression do not see any mental health improvements after trying 2 or more different antidepressants.
Limitations of standard therapies have fueled the growing popularity of ketamine as a treatment option for depression. This rapid-acting substance, previously known only as an anaesthetic, is now actively explored for major depressive disorder and TRD, as well as for anxiety and chronic pain. Randomised trials and meta-analyses suggest ketamine (particularly IV ketamine and intranasal esketamine in approved settings) can reduce depressive symptoms rapidly, often within hours to 24 hours in some patients.
The study led by UNSW and Black Dog Institute in Australia adds to growing evidence of ketamine’s antidepressant effects: response rates among participants grow from 35% at 8 weeks to 44% at 6 months, with improved suicidality scores in 73% of patients. But unfortunately, the effects of ketamine therapy may vary, and the benefits can fade without further treatment.
This article explores how ketamine works for depression and what to expect after ketamine-assisted therapy sessions. Below you’ll find science-based timelines, safety protocols, maintenance recommendations, integration approaches, and a list of possible side effects.
Ketamine therapy for depression: methods and effects
Ketamine was first synthesised in 1962, approved by the FDA for anaesthesia in 1970, and quickly became a popular battlefield medicine. But since the late 1990s, this substance has gained a second life in mental health care thanks to its newly recognised antidepressant properties. Ketamine acts as an NMDA receptor antagonist. Unlike standard ADs, which gradually alter monoamine levels and require 2-8 weeks to build an effect, ketamine blocks NMDA receptors, preventing glutamate binding with them. This temporary “blockade” shifts downstream signalling inside the neuron and forces the processes linked to synaptic plasticity and BDNF activation. In general, NMDA receptors are involved in various neural reactions, where activating molecular mechanisms of BDNF is a key to neuroplasticity — and what makes ketamine so fast-acting.
In ketamine-assisted therapy, the substance can be administered in different ways:
- IV — Intravenous infusions, direct administration in the bloodstream.
It’s the most well-studied, effective, and fast method. Patients receive ketamine through a slow drip over a 40-minute session in an authorised clinic. The substance “flows” straight into the brain. - IM — Intramuscular injections. This method is also effective but, compared with IV, a bit slower. Ketamine first enters small capillaries and only then moves into the bloodstream.
- Intranasal spray — esketamine under the brand name “Spravato”, often provided in clinical settings. Sprays are convenient but less effective, because ketamine must first pass through the nasal epithelium before entering the bloodstream.
- Oral lozenges — common for telemedicine and online-first therapy services. This approach is the least productive: before reaching the brain, the substance passes through the entire digestive system, including sorting in the liver.
Due to its specific mechanism, along with observed rapid antidepressant action, ketamine and its subtypes have become a promising option for people who have already tried several medications without noticeable results. Even in single or low medical doses, ketamine alleviates core depressive symptoms within 2 hours. It produces improvements in mood, cognitive flexibility, and emotion regulation that last for days to approximately 1 week after therapy. These effects make the treatment especially beneficial for patients with TRD and major depressive disorder, who seek rapid relief.
How fast does ketamine work for depression?
Before diving deeper into the effects’ timeline, here’s an important note: the majority of available research covers specifically IV ketamine therapy with repeated administration. This means that timeframes can vary across other, less-studied methods depending on absorption type, dosage, and clinical protocols.
Recent clinical trials show that many patients who tried ketamine infusions notice the first positive effects within 1-2 hours and measurable improvements in depressive symptoms in 1-3 days. Compared to traditional antidepressants, which are usually taken in long-term courses and require weeks to show their efficacy, ketamine creates a striking contrast.
According to several studies, an after-therapy timeline may look like this:
| Time Intervals | Therapeutic Effects* |
| 1-2 hours after the session | Reduced depression symptoms and suicidal ideation, but possible dissociation and an initial “high” |
| 24 hours after the session | Peak of ketamine’s antidepressant effects |
| 1-3 days after the session | Most patients report lasting symptom reduction |
| 1 week after the session | Increased motivation, socialisation, and overall activity, improved cognitive clarity |
| 2-4 weeks (with repeated infusions) | Maintained improvements in symptoms, decrease in depression severity, emotional lift |
| 1-4 months (with repeated infusions) | Stable remission, relief or complete resolution of initial side effects |
| 6-9 months (long-term effects after completing the whole course of infusions) | Some observational follow-ups of repeated/maintenance ketamine report sustained benefit for months among participants who continue treatment and follow-up; outcomes vary and depend heavily on protocol, population, and retention. |
*NB: Long-term figures (months) are less consistent across studies than the short-term (hours–days) effects, and are influenced by whether patients receive ongoing/maintenance sessions and concurrent treatments.
Besides different methods of administration, other factors also influence how effective the therapy is. Response speed is typically linked to the number of sessions, severity of depression, patient’s previous exposure to ketamine, coexisting mental health conditions (such as anxiety or PTSD), preparation procedures, integrative sessions, and how safe the person feels.
How long do the effects of ketamine last?
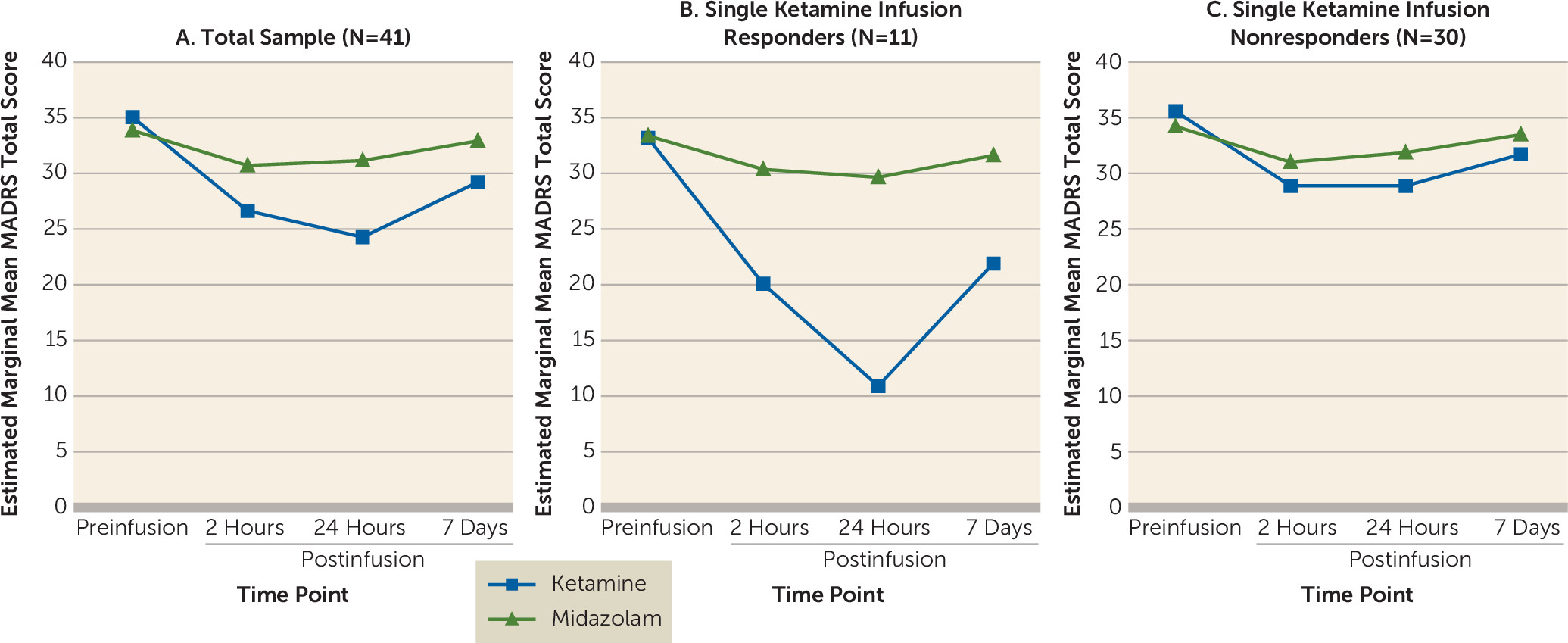
The positive effects can be seen after a single-dose ketamine therapy. A 2020 study found that the most significant reduction of depression scores after a single ketamine infusion was noticed at 24 hours and 7 days after the session. Other studies also confirm that the antidepressant effects of the substance peak at 24 hours. Some individuals report benefits lasting several weeks, but studies on single infusions show the most significant effects within the first 24 hours to 7 days, with relapse risk increasing without further sessions.
Ongoing, multi-dose therapy (e.g., 6 infusions) helps achieve lasting improvement. According to a recent study by UNSW Sydney and Black Dog Institute focused on intravenous and oral generic ketamine therapy, most participants with treatment-resistant depression experienced sustained treatment response within 2-6 months. Depressive symptoms decreased notably during the first 8 weeks and remained stable over subsequent months of repeated therapy sessions. Approximately 35% of patients responded to treatment within 2 months, this proportion increased to 44% by 6 months, while suicidality scores improved in 73% of participants.
In study reports, researchers name the most common post-treatment improvements: reduction in depression severity, depressive symptoms, and suicidal ideation; increased neuroplasticity; improved emotional regulation and mood stability; motivation and socialisation uplift. At the same time, there are still high risks of relapse and, without subsequent sessions, patients may experience a gradual return of depressive symptoms, mood swings, or fatigue.
But why do duration and efficacy vary so much? Several factors can affect the effects:
- Most obviously, treatment protocols: dosage, methods of administration, and number of sessions.
- Severity and chronicity of depression: in severe conditions, therapy may take longer to show noticeable improvement.
- Biological factors: metabolism, individual brain chemistry, genetic and neuroplasticity differences.
- Combination with other therapies or medication: cognitive-behavioural therapy, as well as additional AD treatment, may sustain the antidepressant effects of ketamine therapy.
- Lifestyle factors: nutrition, sleep patterns, physical activity, life stressors, and environment can either boost or slow down possible effects.
- Co-occurring health issues: ketamine therapy shows different levels of clinical efficacy (accordingly, different effects’ duration) for anxiety, PTSD, chronic pain, and other conditions.
Ketamine treatment protocols and duration
Ketamine doses used for depression treatment are significantly lower than those used in protocols for anaesthesia. А 2017 review explains, in IV infusions ketamine is typically administered at a dose of 0.5mg per kg. But in specific cases, the dosage may range from 0.1mg/kg to 0.75 mg/kg, depending on an individual’s response.
Patients receive the substance by intravenous pump during a 40- or 60-minute, carefully supervised session in a clinic after a preparation interview. Many clinical studies and services use a course of ~6 infusions over ~2–4 weeks (often ~2 per week), but protocols vary by setting, patient response, and tolerability.
Repeated sessions help create a cumulative and sustained antidepressant effect. As mentioned above, a single infusion eases depressive symptoms only for up to 1 week at most. For a lasting change, therapy maintenance is necessary. In 2019, researchers compared the effects of single, repeated, and maintenance ketamine infusions and found that, on average, 3 sessions are required to achieve a sustainable response.
Maintenance schedules are not standardised and should be individualised; frequency can range from weekly to monthly depending on benefit and side effects. The authors also note that reductions in depressive symptoms became stable through once-weekly infusions. However, in different trials this frequency was individualised based on participants’ age, health conditions, susceptibility to side effects: from 3 sessions weekly to only 1 session per month.
Another influencing factor is the administration method: they have different evidence bases and monitoring requirements. IV ketamine is often associated with rapid symptom improvement, while intranasal esketamine has trial evidence for use alongside an oral antidepressant and is delivered under structured supervision in approved settings. Long-term outcomes vary and are not directly comparable across studies.
Moreover, the treatment plan depends on its goals. Some patients consider ketamine-assisted therapy as a short-term reset, while others are looking for a long-term solution. Goals should be determined together with your healthcare provider, based on treatment history, symptom patterns, any other medications you take (especially antidepressants), and contraindications.
Safety First: Ketamine Therapy Clinics Carefully Selected by States of Mind
Side effects & safety
Despite promising results, ketamine therapy definitely has its drawbacks: a growing but still limited body of research, a lack of widely accepted safety protocols, and, of course, side effects. Commonly reported adverse effects include:
- hallucinations, blurred vision
- sedation
- temporary dissociation
- blood pressure and heart rate fluctuations
- nausea
- headache
- dizziness
- anxiety
- fatigue
The duration of side effects depends on how quickly ketamine is metabolised in the body. The substance’s half-life is typically 2 to 4 hours, so acute side effects mostly resolve within this time period. To mitigate and prevent adverse experiences, authorised clinics provide continuous monitoring and trained medical supervision during each session, as well as carefully controlled dosing.
When ketamine therapy may not be appropriate
Since ketamine can increase blood pressure and heart rate, clinics typically screen for cardiovascular risk and monitor vitals during and after dosing. Patients should not drive, operate machinery, or make high-stakes decisions until fully recovered and cleared by the treating service.
It’s also worth noting that not all patients are eligible candidates for ketamine therapy. Ketamine may be unsuitable for some people and requires careful screening. Many clinics treat active psychosis (or a history of psychotic disorders) as a strong contraindication; substance use disorder, pregnancy/breastfeeding, and significant cognitive impairment often require specialist assessment and may preclude treatment depending on risk. Eligibility criteria vary by service and jurisdiction.
Ketamine therapy and integration
Experts suggest, psychotherapy can multiply ketamine’s benefits for mental health. While ketamine for depression works on a molecular level, rapidly enhancing synaptic connectivity and increasing neurobiological receptivity, talk therapy may facilitate extended cognitive and emotional restructuring. In other words, KAT creates a unique window for change, and psychotherapy helps reinforce new pathways for a deeper effect.
Different integration approaches balance ketamine sessions with trauma-informed therapy or cognitive-behavioural therapy (CBT) after each visit, provide psychoeducational preparation before the first day of treatment, and maintain behavioural activation therapy to prevent relapse of depressive symptoms. Moreover, adjustments in the medication plan (only after consultation with your therapist) can also support long-term stability.
But integrative therapy doesn’t stop at the clinic door — it lives on in your daily rituals and habits. Self-care is a powerful booster of the healing process. Small everyday routines, such as regular work-outs, sufficient sleep, healthy meals, reduced drinking, stress management, and self-compassion, reinforce the positive changes from therapy.
Ketamine therapy is gaining momentum worldwide. It’s drawing attention within the medical community, creating a buzz in international media, and sparking lively debate on Reddit. With new ketamine clinics opening in Europe and beyond, KAT is steadily solidifying its place as a legitimate, research-supported option for severe and treatment-resistant depression. Nevertheless, clinical data are currently limited, so this type of therapy should be approached with caution, from both medical providers and patients.
If you’re considering ketamine therapy, start by booking a consultation with a qualified specialist to understand eligibility criteria, timelines, potential effects, costs, and integrative therapy options. For more information, check out this list of providers and take our online assessment to find out whether ketamine therapy might be the right fit for you.



















































