Reading Navigation
Ketamine Vs. Psilocybin Therapy: The Difference in Treatment
Ketamine therapies have been FDA-approved in the US for just shy of a decade, and as a result, there has been a rapid increase in clinics offering these ketamine-based treatments. In fact, the esketamine nasal spray (ESK) has been approved for use in around 78 countries worldwide; though recreational use is mostly illegal.
One byproduct of this rise in popularity has been the growing interest around psychedelics-based therapies too. However, psilocybin is currently illegal in most countries, due in part to the UN 1971 Convention on Psychotropic Substances classifying it as a Schedule I substance. However, as more countries have reformed their drug laws, things have begun to change. As it stands, psilocybin is: *
- Fully legalised: Jamaica, and the Netherlands
- Legal to possess and use, but not sell: The Bahamas, and in the British Virgin Islands
- Legal for medical use: Australia, New Zealand, Canada, Czech Republic, Germany, and Switzerland. In the US it’s been legalised in Oregon and Colorado (with New Mexico soon to come)
- Decriminalised: Portugal, Spain, Costa Rica
- Religious exemption: Mexico
That said, owing to the relative “novelty” of both, it can be difficult to first understand what these kinds of therapies involve, and secondly how they work. Furthermore, while they do share some similarities, understanding just how fundamentally different these treatment options actually are can be complicated. Therefore, this article seeks to provide a balanced overview of both therapies, along with evidence-based comparisons in order to help you stay informed.
| * Medical Reviewer’s Note: Psilocybin legalisation |
| The legal status of psilocybin involves highly specific regional frameworks rather than blanket legalisation. In the Netherlands, psilocybin mushrooms are banned, but a legal loophole permits the use of psilocybin-containing ‘truffles’. Jamaica operates in a permissive gray area lacking explicit prohibition. Medically, access is highly restricted globally: Australia permits prescribing solely by authorised psychiatrists for treatment-resistant depression; the Czech Republic will implement a framework for limited psychiatric prescription starting in 2026; and countries like Canada, Germany, and Switzerland restrict access strictly to specialised compassionate use or special access programs. |
What Are Ketamine and Psilocybin?
Ketamine is a dissociative anesthetic synthesised for medical use in 1962 as a safer and faster-acting alternative to phencyclidine (PCP). PCP had been used as a general anesthetic since the 1950s but was discontinued due to post-operative dysphoria and hallucinations.
Following successful medical trials, ketamine was approved by the FDA in 1970 for veterinary and human use — the first being on American soldiers during the Vietnam War. From here, more research into ketamine’s therapeutic uses was conducted. However, its growing popularity also caused a growth in illicit use, and so it was promptly made a controlled substance in 1999 in the US.
Psilocybin, on the other hand, is a naturally occurring psychedelic compound found in psilocybin mushrooms or “magic mushrooms”. It has a hallucinogenic effect and can be obtained from fresh or dried mushrooms; their use has a long history in traditional ceremonies across almost all continents.
As of right now, psilocybin is illegal under US federal law in all but the two aforementioned states. Additionally, there is a growing body of research that points towards its potential usage in the clinical treatment of substance disorders and other mental illnesses. This trend has also been seen on the global stage, with many countries across the world beginning to expand their scientific inquiry into the medical use of both substances.
How Do They Work in the Brain?
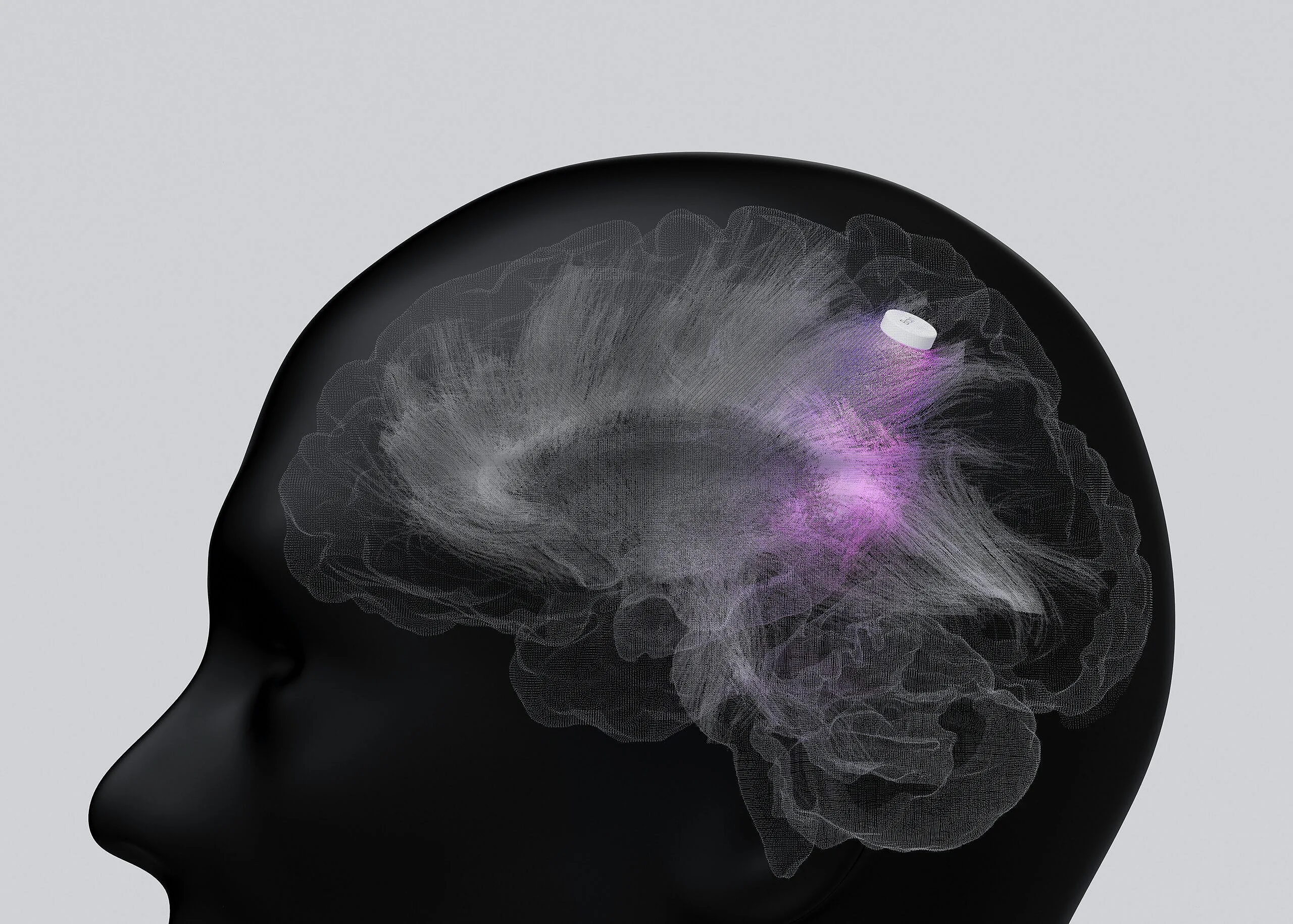
Ketamine binds to the N-methyl-D-aspartate (NMDA) receptors in the brain. Acting as an antagonist (at antidepressant doses), this localised blockade triggers a surge of glutamate to be released in the prefrontal cortex. Glutamate is an abundant and vital neurotransmitter found in the nervous system that provides a range of functions, such as pain transmission, mood regulation, and learning and memory regulation. It’s also been found to work as a chemical messenger, a sleep mediator, and an alternative energy source for the brain when glucose levels are low. As a result of this burst of glutamate, AMPA receptors are activated, which stimulates the neurotrophic pathways that promote the growth of new neural connections.
In contrast, psilocybin is a serotonin receptor agonist that primarily targets the 5-HT2A receptor. The psychoactive and hallucinogenic properties of psilocybin are directly driven by its active metabolite, psilocin, acting as a partial agonist at serotonin 5-HT2A receptors. Serotonin is a neurotransmitter responsible for mood and emotional processing, digestion, and sleep. Thus, the initial serotonergic activation, and downstream interactions with the glutamatergic system help facilitate the long-term neuroplasticity associated with psilocybin’s sustained antidepressant effects. Hence, it’s shown potential for the treatment of mood and anxiety disorders, and found to offer pain-relief in various clinical studies.
| Spotlight Section: Glutamate |
| There is a growing body of evidence that points towards glutamatergic dysfunction playing a role in many major psychiatric disorders — such as MDD, bipolar disorder, and schizophrenia. The therapeutic potential of both substances is, therefore, thought to come from glutamate modulation. |
What Conditions Are They Commonly Used for?
Ketamine and psilocybin have both had a long history of clinical and recreational use. However, owing to the different ways they work on the brain, their therapeutic usage varies. For instance, ketamine these days is used medically for treatment-resistant depression, managing suicidal ideation, and pain management — like fractures, trauma, extremity pain, lower back pain, and abdominal and flank pain. Ketamine has some off-label uses as well.
For example, during emergencies it’s used to provide short-term sedation and rapid sequence intubation — this is when a sedative and neuromuscular blocking agent (muscle relaxant) are given simultaneously to quickly induce unconsciousness and paralysis. Furthermore, emerging research is also looking into its utility and efficacy in treating refractory status epilepticus (RSE) — a life-threatening condition where seizures fail to respond to first- and second-line treatment options; although, this is still awaiting FDA approval.
On the other hand, the first recorded use of psilocybin mushrooms is thought to date back as far as the early 1500s CE. This consumption is believed to have been for ritualistic and spiritual purposes, due to their hallucinogenic properties. In the modern era, psilocybin’s legal status has limited clinical use. Clinical research has indicated its efficacy in treating mental health conditions like obsessive-compulsive disorder (OCD), anxiety and depression, major depressive disorder (MDD), PTSD, and substance use disorders. There is also emerging exploratory work being conducted on the integration of psilocybin-assisted therapy for individuals with palliative care needs.
| Spotlight Section: Neuroplasticity |
| Neuroplasticity (or brain plasticity) refers to the brain’s ability to change, adapt, and make new connections in response to new experiences or new information. “It’s a term that all these substances share, whether it’s ketamine or psilocybin”, says Dr Sam Zand, DO, holistic psychiatrist and founder of Anywhere Clinic. “Creating new neural networks in the brain fertilises it, which leads to new pathways, emotions, and behaviours. So you’ll have people who’ve tried therapy and other methods all of a sudden say they feel ‘unstuck’. It lubricates the mind, and whatever patterns they were previously in feel easier to deviate away from”, he finishes. |
What Does Each Therapy Feel Like?
Ketamine Therapy
Since the FDA approved Spravato (esketamine) in 2019 for the treatment of treatment-resistant depression, there has been a growing inquiry and acceptance of ketamine therapy by the public. In fact, Dr Zand has a funny story on this exact topic: “I once had a patient who came to my practice around that time, and he told me how he decided to leave his previous psychiatrist because they kept trying to give him ketamine”. He continues, “he said to me, ‘at the time I thought it sounded reckless because I didn’t really understand the molecule. But now that it’s approved, it changes my whole perception around it’”.
Nevertheless, despite its increasing popularity, many are still curious about how it works. In short, ketamine therapy is done through different methods. “These approaches include: an IV, an intramuscular injection in the shoulder, an in-clinic intranasal spray, or an oral lozenge for home use”, Dr Zand states.
On low doses, ketamine therapy feels meditative, relaxing and sometimes euphoric, though Dr Zand has found that it’s even better on the nervous system when patients practise breath work and journaling before. “You’ll be going through a little bit of a mind-altering experience during this time, so it’s key to calm your mind and body. This enhances that, so it becomes a medication-enhanced meditation”.
On average, the experience lasts around 30 minutes, and at most two hours. When it comes to how it feels, his patients report different things. Though, the general descriptions tend to summarise it as an internal dissociative experience. Experiences are often less visual; however, this can change on higher doses.
“At higher doses it can become a little psychedelic because of the mind-expansive properties [of ketamine]. So it can sometimes create subconscious projections that we can visualise. Others describe themselves flying or swimming on these higher doses too”, Dr Zand says. As a result, he generally recommends eye masks, headphones, and soothing meditative music to facilitate the inward journey. “There’s a wide range of experiences, but the best way to go through it is with a good therapist, and especially afterwards, to do a bit of therapeutic work to mould the mind while it’s still flexible”, he finishes.
Psilocybin Therapy
“With psilocybin therapy, it’s a similar concept, similar preparations, intentions, and in some cases similar desired outcomes. However, the main major difference is that the psilocybin experience lasts longer. So, instead of it being a short one-hour experience, it can go on for three to five (sometimes up to eight) hours. This can be difficult to contain in a safe way, and getting a therapist or clinician for the entire duration has the potential to become very expensive. Therefore, ketamine therapy is clinically more accessible and affordable”, Dr Zand explains.
The experience is often immersive and emotionally intense. People who do this kind of therapy do it in order to expand the mind or to gain clarity on whatever ails them. For example, they may also be looking to gain a different perspective on themselves, their life stress, relationships, or any conflicts they are experiencing. Others often do it as a means to further assist any therapy or medical treatment they’re already going through. “They may want to soften their approach to self, and to create a little bit more empathy and understanding so that they’re more self-aware and not just being reactive”, Dr Zand says.
The Effectiveness and Longevity Benefits of Both
As mentioned above, ketamine therapy tends to have a rapid onset that leads to shorter session length. In addition, the duration of treatment varies, though multiple sessions are often required. Nevertheless, various studies have indicated very promising results for the treatment of treatment-resistant depression.
“We have good evidence that looked into people who’ve tried therapy and antidepressants before. When they started Spravato treatments alongside a (newly initiated) oral antidepressant, patients with treatment-resistant depression demonstrated significant improvement. Response rates — defined as a 50% or greater reduction in symptom severity — ranged from 50% to 70%, with strict clinical remission rates reaching between 30% and 52%”, Dr Zand explains. In addition, the FDA has recently approved its use as a monotherapy (the use of a single drug or method for treatment) — a move that’s further expanded its clinical utility.
As for the general treatment length Dr Zand sees in his patients, it varies. For those who began treatment as high-risk patients (reported to feeling suicidal prior to treatment), for instance, it’s safer to stay on the treatment long term with sessions continuing every 1-2 weeks. In contrast, patients whose symptoms are less severe will usually stop treatment and replace it with close monitorisation.
As for psilocybin therapy, there is less need for multiple treatments. “There are interesting studies that have indicated that just a single dose of psilocybin was enough to make a profound change in some individuals. However, the reasons for this still need to be explored. But, in my (personal) opinion, I think the perception and paradigm shift that happens creates a creative spark or desire to see parts of ourselves in different ways of some permanence”, Dr Zand shares. He likens the neuroplasticity benefits of psychedelic drugs to ‘warming up the clay of the brain’, which in turn creates a fertile environment for changes to be made.
This effect may be further heightened by the communal environment psilocybin is taken in. “There’s a connectivity with nature and other people. People can also move around and walk safely — in fact, many discuss experiencing a restlessness that is helped by doing so”, Dr Zand says. With ketamine therapy on the other hand, individuals will need to be laying down on the couch or bed for the sessions, and are even advised to not move around too much. “So, maybe there’s something about the immersion with nature that brings our mind back into harmony”, he finishes.
There’s a very famous quote that says, “Psychedelic medicine is to psychiatry, what the microscope is to biology”. So, I think what we’re looking at is the paradigm shift in mental health — from treating the symptoms and focusing on downhill symptomology to going upstream and examining what’s at the core. I think questions like, “How do I change my subconscious patterns?”, and “How do I truly get to know myself so that I can not only find self-acceptance and self-love, but also understand which levers to pull?” are at the heart of this shift in awareness.
Dr Sam Zand
Risks, Side Effects, and Safety Considerations
“In general with ketamine and psilocybin, it’s important to make sure that you have good cardiovascular health and that your blood pressure isn’t elevated. But with ketamine specifically, you need to be well hydrated and have good bladder health”, Dr Zand advises. There are also recreational risks, though these can be mitigated in the right context. Other potential side effects include nausea, vomiting, dizziness, dissociation, confusion, and double vision (diplopia).
In contrast, the most commonly reported side effects of psilocybin are headaches, anxiety, nausea, dizziness and elevated blood pressure levels — although, these appear to be at tolerable levels for most and resolvable within 48 hours. Additionally, the psychedelic effects can also lead to emotionally intense experiences that cause psychological distress, in some cases.
Lastly, both ketamine and psilocybin therapy have raised concerns around misuse and their long-term safety — particularly when it comes to pediatric psychiatry. However, as it stands, more research is needed to ensure a thorough risk-balance assessment. But in the meantime, screenings, medical supervision, and therapeutic support are essentials for both therapies.
| Spotlight Section: Psilocybin and Serotonin Syndrome |
| It’s important to note that while patients were historically advised to taper off standard antidepressants before psilocybin therapy due to theoretical concerns regarding Serotonin Syndrome. Recent comprehensive reviews have indicated that combining SSRIs with psilocybin may in fact be generally safe. This is because psilocybin acts directly as a receptor agonist rather than a serotonin-releasing agent — making the risk of toxic serotonin overload exceedingly low. As it stands, the primary clinical interaction observed is that chronic SSRI use causes receptor downregulation, which may significantly blunt the subjective intensity of the psychedelic experience. |
Ketamine vs. Psilocybin Therapy: How to Choose?
The legal status of both substances varies quite considerably. As a result, different countries, territories, and states will have differing requirements and restrictions for each therapy. In general, these regulations are based on the law (international or otherwise), as well as medical and pharmacy boards.
Nevertheless, should you live in a place where they are both legal, their applicability for you will depend on a few different factors. These include:
- Doctor’s discretion: In order to work out if either of these therapies are suitable for you, your doctor will consider things like your medical history, your tolerance level for being in altered states, and whether or not you need/want rapid symptom relief or a deeper, more self-exploratory therapeutic experience.
- Practical considerations: In addition, it’s vital that you also weigh the pros and cons for each therapy. You should think about the availability of the programs, their accessibility of the clinics (this includes the time you can commit to them as well as things like travel), the financial cost of each (self pay, insurance, or both?), your emotional state, and your readiness for each/either experience.
- Ethical considerations: In order to supplement research, you might want to have a look into ongoing clinical trials, as well as review previous scientific studies into each therapy. After all, both ketamine and psilocybin therapy are growing in popularity, and so their applicability for medical use is likewise a growing field of scientific inquiry. More than anything, this approach will ensure that your decision is informed by evidence-based practice and not hype.
The utilisation of ketamine and psilocybin (and psychedelic medications in general) indicates some potential for their unique application as therapies. As Dr Zand emphasises, “in psychiatry, we’re very excited about the ability to use these substances safely and medically”. However, many things still need to change in order for undergoing these various therapies to be okay.
“There are a lot of professions — for example, first responders, nurses, police officers, firefighters, military personnel, and teachers — who aren’t allowed to seek these emerging treatment options. So, safety is still important, but we also have to change our approach and guardrails a little bit too”, Dr Zand adds. Nevertheless, this article should have equipped you with enough information to aid your understanding of them.