New Solutions for Anorexia: Expanding Conventional Therapy

Eating disorders, especially anorexia nervosa (AN), are severe mental health conditions. Standard psychological treatments for anorexia — talk therapy, meal plans, and medication —may be helpful for sufferers. Yet 40–50 % of patients with diagnosed anorexia slide back into disordered eating behaviours within months of discharge. Besides this, AN carries the greatest mortality risk of any mental illness, with higher rates of suicide than depression.
Researchers are now testing whether psychedelic therapy can open a fresh path to recovery. Among the most promising of these substances is psilocybin, which is found in “magic mushrooms”.
Psychedelics Reframing The Treatment
Anorexia nervosa (AN) is more than refusing food — it can be conceptualised as a powerful psychological loop of perfectionism, fear, and self‑criticism. Traditional treatments, including cognitive-behavioral therapy and nutritional counseling, have helped many, but relapse rates remain high.
This has sparked worldwide interest in psychedelics as a treatment for anorexia nervosa, asking: could one big shift in mindset start a new recovery track? Supporters see these medicines as tools to knock down the “brick wall” of rigid thinking that talk therapy sometimes cannot penetrate. Laboratory research shows that psychedelic substances can boost brain plasticity mechanisms and create a window for change — and that therapeutically these processes can be harnessed to establish new connections and reconsider familiar patterns.
However, it’s important to note that most studies on psychedelic-assisted therapy for eating disorders are now in the very early stage of research, undergoing Phase 1 feasibility trials.
How Does Psilocybin Therapy for Anorexia Work?
Recent studies describe a three step psychedelic therapy process for eating disorders:
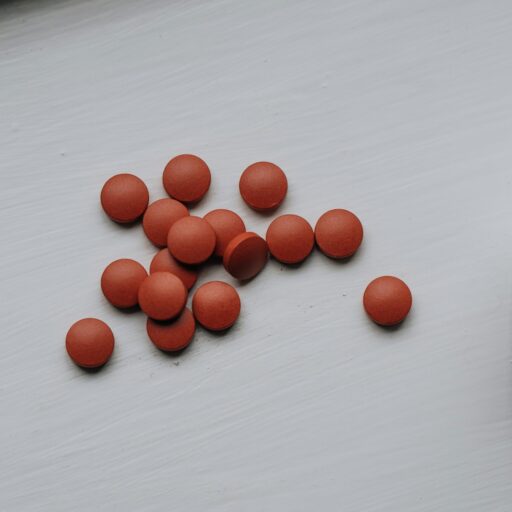
- Preparation sessions: A client meets guides, sets goals, and then undergoes several of check-ups, screenings, and blood tests.
- Dosing day: In a calm room, after breakfast, a client takes a controlled dose of psilocybin and turns attention inward for the next eight hours. Psychologists and guides stay close for support during the whole day.
- Integration: The morning after, a client shares insights with the study psychologists in a one-hour integration session. Over the next three months, all patients will be supported in adapting their eating routines and reviewing their habits.
Integration is the heart of psychedelic-assisted therapy: not the drug alone, but in combination with guided change. Brain scans show the psilocybin sessions spark a short “neuroplastic window”, when old thought‑loops soften and new habits can take hold — one reason advocates link psychedelics and anorexia recovery.
First Results of Psychedelics Trials
Small psilocybin clinical trials for anorexia nervosa show promising stories — one or two guided sessions can spark a vivid shift in self‑perception. Participants describe meeting their harsh “inner critic” and letting it go; many feel a sudden, compassionate view of their bodies, as if looking through kinder eyes.
4 out of 10 respondents showed clinically significant improvements in their anorexia nervosa symptoms. But perhaps more importantly, the quality of their experiences was profound:
- 90% felt more positive about life
- 80% ranked the experience among the top five most meaningful of their lives
- 70% reported a fundamental shift in their sense of identity
- Early numbers suggest anxiety drops and food rituals ease for weeks afterwards
Overall, these early signals place psilocybin for anorexia nervosa at the centre of modern research. Scientists now aim to confirm whether the burst of mental flexibility observed in pilots can translate into long‑term freedom from food rules.
Microdosing Insights
In 2023, researchers from the University of California, San Diego, published the first modern clinical trial examining psilocybin for anorexia nervosa. The small but significant study followed 10 women through a designed protocol. It involved a single dose of psilocybin combined with psychological support.
“Genuinely the most healing experiences every time,” shares one of the participants. “My first trip with psilocybin is seriously what healed my suicidal thoughts and some traumas, and each time after, I healed more and more. It’s significantly improved my mental health faster than anything else. Even though it’s only taken once or twice a year. Incredible.”
Most of the participants (90%) self-reported positive changes within three months after the dosing. Early results suggest that such therapy increases emotional openness, reduces obsessive thinking, and even softens rigid self-beliefs. “It puts you back in touch with what’s beautiful about the world and people. It can be an incredibly moving, kind of connecting thing”, the respondent notes.
Who Might Try Psychedelic Therapy for EDs
If you’re considering this type of therapy for anorexia nervosa, the researchers have put together several recommendations for potential participants. Relevant candidates are adults, 21-65 years, with a diagnosis of AN for more than 3 years, who have tried regular care first. They need stable heart tests, to not be taking contraindicated medications like some antidepressants, balanced electrolytes, and medical supervision. People with psychosis, uncontrolled heart disease, or very low BMI should avoid psychedelic sessions for now.
Licensed centres for psychedelic-assisted therapy, which are currently located only at universities, medical offices and clinical research centers, follow strict safety plans so that AN treatment remains as safe as possible.
Find Therapeutic Support That Matches Your Needs
Other Psychedelic Options for Anorexia Nervosa Treatment
Treatment options for anorexia nervosa are gradually shifting beyond traditional talk therapy and appetite-stimulating medications toward approaches that target the brain’s underlying mechanisms. Current research is exploring how to modify rigid thought patterns, enhance cognitive flexibility, and address the neural circuits involved in reward, control, and self-perception.
Ayahuasca
In terms of other psychedelics, ayahuasca also presents significant improvements in emotional regulation and processing. Compared to other eating disorder treatments, it enables deeper healing via a spiritual component and can become the next antipsychotic drug for anorexia nervosa.
MDMA
Well known as an “empathy booster,” MDMA is now being tested for addressing self‑critical thoughts. MDMA boosts serotonin, dopamine, noradrenaline and the bonding hormone oxytocin, which may soften harsh self‑talk and boost self‑compassion — frequent companions of anorexia. Small case reports and a 2024 scoping review note fewer restrictive thoughts after two MDMA‑assisted sessions.
Ketamine
Ketamine is a dissociative anaesthetic that acts rapidly on glutamate signalling pathways, lifts low mood, and “resets” reward circuits that treat food restriction like a win. Case series of group-based ketamine-assisted therapy found weight gain and reduced food anxiety four weeks after three ketamine sessions. Larger trials are in planning.
Several clinical trials are underway to evaluate whether new pharmacological agents and adjunctive therapies can complement psychotherapy and provide more effective, lasting outcomes for people with anorexia nervosa.
For instance, the Centre for Affective Disorders at King’s College London is running clinical trials on psychedelic therapies such as psilocybin, 5-MeO-DMT, and MDMA to assess their safety and effectiveness in conditions like treatment-resistant depression and PTSD. Alongside testing, the team is developing therapist training and healthcare models, supported by a mix of public and private funding. In 2022, it launched the Centre for Mental Health Research and Innovation in collaboration with key partners to accelerate this work.
Ongoing Research of Psychedelic-Assisted Therapy
As research on psychedelics for anorexia nervosa continues, the goal is to expand the therapeutic toolkit. Several ongoing clinical trials can become a breakthrough in anorexia nervosa therapy:
- Large-scale study at Imperial College London, treating anorexia nervosa with psilocybin;
- Study at Johns Hopkins University, observing how depression with chronic anorexia could be relieved with psychedelics;
- Study by the pharmaceutical company COMPASS Pathways, comparing the efficiency of microdosing with psychological support, to treat anorexia nervosa.
But like any therapy, psychedelics aren’t a silver bullet for treating anorexia. They work best alongside nutrition plans, family support, psychological treatments, and skills practice. For hungry minds, it offers something that calorie counting never could: reconnection and escape from harmful patterns.