Reading Navigation
What Does a Manic Episode Feel Like?
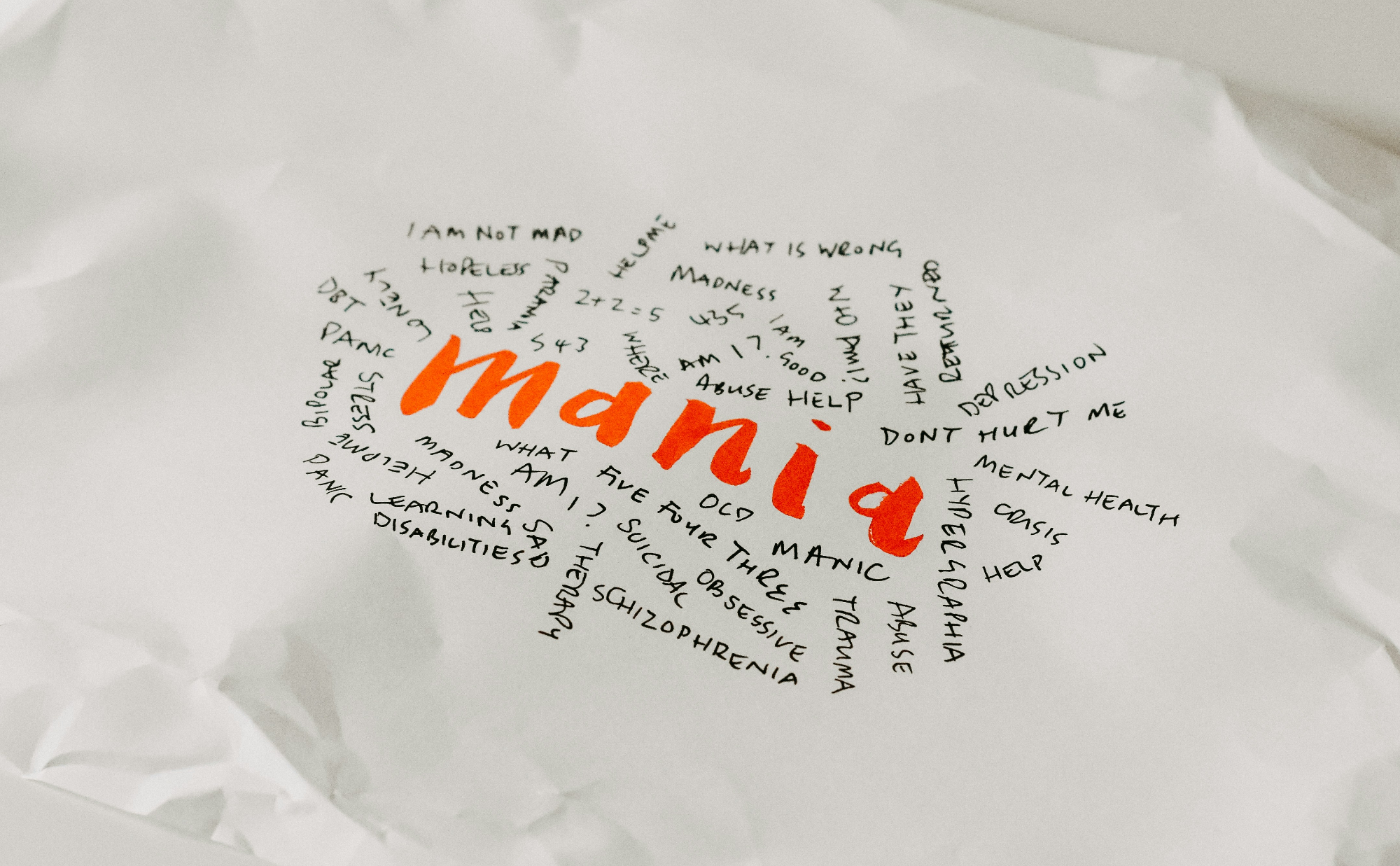
A manic episode is a challenging experience that can leave you and the people around you feeling overwhelmed, stressed, and confused. During a manic episode, you may feel like1 your mind is racing uncontrollably, and your energy is high. You feel overly excited and start attaching a high degree of urgency to things that aren’t necessarily urgent. You may feel powerful or invincible, get very little sleep, and act in ways that are out of character.
Manic episodes (also called mania) can affect about 4%2 of the general population. Mania is a core feature of bipolar disorder, particularly bipolar1 I disorder. If you have received a diagnosis of bipolar I disorder, you might experience from 1 to 2 manic episodes3 in your lifetime. to multiple episodes in a year, depending on factors such as individual vulnerability, exposure to triggers, and consistency of treatment and medication adherence.
It is important to understand what mania feels like because the early signs are often missed. You may not feel2 that your behavior is out of the norm, and the signs may be mistaken for productivity, confidence, or even other mental health conditions4 like ADHD and PTSD.
Recognizing the early signs of a manic episode helps ensure you, or others, get the appropriate treatment and support and can help prevent risky decisions, accidents, harm to relationships, or escalation of the episodes.
What Is a Manic Episode?
A manic episode1 is a period of unusually high energy and extreme changes in mood and emotions, behavior, and general activity level, which can often be noticed by friends and family and lasts for at least a week1.
During periods of mania, people tend to experience a sustained feeling of high energy, irritability, restlessness and reduced need for sleep, racing thoughts, and euphoria. Others may also experience hallucinations and disorganized thoughts. These feelings can significantly affect daily function, leading to risky or impulsive behaviours with long term repercussions and, in some cases, may require receiving medical care.
A manic episode is a hallmark characteristic5 of bipolar I disorder. Mental health professionals use its symptoms as diagnostic criteria to determine whether or not a person has bipolar I. On the other hand, a hypomanic episode, also called hypomania, is the hallmark characteristic1 of bipolar II disorder.
Mania and hypomania are both characterized by higher-than-usual levels of energy, mood, and behavioral changes; however, they differ in intensity and severity.
During hypomania, you experience less severe manic symptoms that often don’t cause major impairments to daily functioning. This is in contrast to mania, which causes more severe symptoms and complications. Also, a hypomanic episode typically lasts for a shorter duration (about four days), unlike a manic episode can last longer.
How Long Does a Manic Episode Last?
The length of a manic episode varies from person to person, but a criterion is that it should last at least one week1. It can last for months6 for some people and longer than a year7 if untreated.
Aside from not getting adequate treatment, there are several reasons why an individual may experience a longer duration of mania or more intense episodes, including:1
- Sleep deprivation
- Substance use
- Changes in daily routine
- Experiencing stressful life events
- Having other coexisting medical conditions, such as personality disorders and trauma
Mania typically does not stop occurring without treatment. This is because it is not just a temporary change in mood or emotions. Rather, it is a symptom of a chronic brain condition that can progress over time. A 2023 review8 of brain imaging studies shows that bipolar disorder is associated with structural changes to certain parts of the brain, particularly the prefrontal cortex9, which is involved in emotions, self-control, and decision making. The authors also highlighted that preventing manic episodes can prevent neurological changes increasing in severity.
Common Signs and Symptoms of Mania
Mania can cause remarkable physical, behavioral, and emotional symptoms7, which can range from mild to debilitating10.
Physical and Behavioral Symptoms
Symptoms that people can usually notice when you are experiencing a manic episode include:
- Markedly increased energy and the need to get involved in goal-directed activities
- The need to carry out tasks urgently
- Feeling like there is a decreased need for sleep, without feeling fatigue
- Talkativeness
- Agitation or constant movement
- Disruptions to routine
- Rapid, pressured, or excessive speech
- Impulsivity and risk-taking (e.g., spending unnecessarily, sex, substance use, reckless decisions)
- Change in appetite
Mental and Emotional Symptoms
Your mental and emotional health would be impacted, and you may experience:
- Racing thoughts or “ideas jumping ahead”
- An inflated self-confidence or grandiosity
- Elevated, expansive, or unusually irritable moods
- High sensitivity and emotional reactivity
- Feeling of unease and nervousness
- Difficulty focusing or sustaining attention
- Instability and change in energy from moments of “high” to moments of “low”
Severe or Dangerous Symptoms
A severe case of mania can present with:
- Psychotic features1 (delusions, hallucinations)
- Suicidal thoughts
- Loss of insight or inability to recognize the symptoms of mania as they occur
- Excess involvement in reckless activities or behavior that poses a risk to oneself or others
What Does a Manic Episode Feel Like?
When experiencing a manic episode, you may not be aware — and you are not alone in this, as many people with this condition don’t recognize when an episode is coming. Contrary to what you may think, the start of a manic episode typically does not feel unpleasant. Instead, people have described it with words like11 “pleasant,” “enthusiastic,” “pleasure,” and “fascination.”
A manic episode can feel pleasurable at first with a rush of energy and racing thoughts, followed by some strange feeling of unease, extreme irritability, or agitation. You may also want to look out for feelings of being all-powerful11, invincible, more intellectually sound or intelligent than others, and feeling that you are on top of the world and can do anything.
Amidst these feelings and waves of emotions, a manic episode can be dangerous because the feelings don’t exactly reflect reality. For instance, some people experience grandiose delusions12 in which they see themselves as someone with uniquely exceptional abilities, such as a hero, a secret service agent, or even receiving messages from a spiritual being or god. At such an emotionally high moment, you are prone to taking irrational decisions and acting erratically, e.g., drinking excessively and driving under the influence of alcohol.
How Mania Appears to Others
Most people don’t recognize when they are having a manic episode. This is understandable because during a manic episode, your sense of judgment is impaired, and you have little to no insight or control over your emotions and behavior.
But your family, friends, and close colleagues at work are often able to identify a manic episode when you are having one. They may notice early warning signs like:
- A change in the way you communicate, e.g., constant domination of conversations, interrupting others when they are speaking, and making grand claims
- A deviation from your usual behavior, e.g., you act impulsively and take erratic decisions
- You talk unusually fast
- You set sudden, unrealistic goals
- You act with a high degree of urgency
- You display intense or unwarranted anger and get easily irritated
The Aftermath: What Happens After a Manic Episode?
After the rushing feeling of elation and excitement that occurs during a manic episode, there may be a period of vagueness or dissociation11 where it appears you do not remember things that happened.
Some people enter a phase of exhaustion6, which is considered a possible transition into major depressive episodes. You may feel emotionally and physically crushed. Feelings of regret, shame, guilt, and confusion may also occur at this stage11.
An older study13 that followed up a small number of people with bipolar I disorder six months after a manic episode found that most of them experienced mood and cognitive symptoms for about half of the follow-up time.
Many people, after a manic episode, come to terms with reality and now deal with the painful impact of the episode. This includes damage to different aspects of life, such as finances, social life, or relationships. This may trigger depressive symptoms11, such as:
- Sadness and anhedonia
- Feeling of lethargy
- Difficulty focusing or remembering things
- A feeling of emptiness
- Lack of desire to participate in day-to-day activities, such as work
- A feeling of hopelessness, shame and inadequacy
It can be challenging to manage the wave of emotions, but it’s important to extend kindness to yourself and understand that recovery is a gradual process. Aside from reducing your symptoms, wholesome recovery also includes rebuilding, restoring stability, and reducing the chances of another episode occurring.
When to Seek Help
It may be difficult to know exactly when to seek help if you are experiencing a manic episode. But an intervention is necessary and important, particularly when your symptoms are escalating, to prevent causing harm or engaging in risky behaviors.
Here are some red flags that require you to seek urgent help for yourself or your loved one:
- Signs of hallucinations or delusions, e.g., hearing, feeling, or seeing things that are not there
- Depression symptoms, e.g., a prevailing sense of sadness, doom, and hopelessness
- Suicidal thoughts
- Intense agitation or extreme irritability
- High-risk behaviors like reckless driving, gambling, or excessive spending
- Inability to function at work or school
Symptoms like these should prompt calling emergency numbers like 911 or the suicide and crisis lifeline. Milder symptoms like sleep disruption, changes in mood and energy, relationship issues, and difficulty focusing may not require calling an emergency number. But it still helps to contact a mental health professional to lower the chances of escalation.
Support Is Just A Click Away
Supporting Someone Experiencing Mania
People experiencing mania can benefit greatly from support from family and friends. If you are wondering how best to support someone going through a cycle of mania, here are things you can do:
- Reach out to them and communicate with love.
- Lend a listening ear. Offer them a safe space to share how they are really feeling.
- Try to understand that they are dealing with a condition they have little to no control over, so show compassion.
- Encourage them to care for themselves by adopting healthy lifestyle habits and getting appropriate medical care.
- Set healthy boundaries.
- If issues or conflicts arise, try to stay calm through it while pointing out when they have done something that isn’t acceptable.
- Gently let them know about any warning signs you may have observed.
- Avoid making statements that may lead to feelings of shame and self-blame.
- Avoid being overly confrontational or judgmental.
- Encourage them to get professional help and help them stick to their medication schedules.
Treatment and Long-Term Management
Conventional treatments for bipolar disorder and its symptoms include medications, talk therapies, and outpatient programs.
Medications
Healthcare providers typically prescribe mood stabilizers2 like lithium and carbamazepine or antipsychotics like risperidone and haloperidol. Anticonvulsants can also be effective for stabilizing mood; however, they are not considered as effective7 as mood stabilizers and antipsychotics. Sometimes you may need to take a combination of medications in these classes.
Note: Bipolar depression treatment is not the same as unipolar depression (like major depressive disorder). Standard antidepressants have been thought to increase the risk of mania (although recent studies14 indicate that this risk is lower than previously believed)
Therapy
Psychotherapy is a powerful tool for managing bipolar disorder. Also called talk therapy, psychotherapy15 involves structured conversations with trained mental health experts to help you identify, manage, and resolve unhealthy emotions and troubling thoughts and behaviors.
Therapy can help you manage depression and anxiety symptoms, which are both common and co-occur with bipolar disorder. It is recommended for stress management and can improve your emotional and psychological well-being.
Therapy sessions can also be helpful for managing sleep disturbances, which are very common among people with bipolar disorder and have a detrimental impact16 on recovery, treatment outcomes, and quality of life. A therapist can guide17 sleep-behavioral changes and challenge any unhelpful beliefs you may have about sleep, e.g., a belief that hitting your bed early won’t help you fall asleep anyway.
Lifestyle changes
Because bipolar disorder is a chronic condition, long-term sustainable strategies are essential for managing symptoms. Studies indicate that the risk of suicide is more than 10 times higher among people with bipolar disorder than among the general population.
Here are 10 things you can do to reduce the risk of relapsing and to promote overall health and wellness:
- Try to get at least 7 hours of sleep per day. Sleep can improve depressive symptoms. You can try doing things that can help regularize your sleep and wake times, such as relaxing towards bedtime, using sleep-supporting night lights in your room, minimizing screen time, and setting alarms.
- Relax more and reduce your stress level. Stress is considered a major risk factor for bipolar disorder18.
- Take breaks from news and social media, and make time to relax and unwind.
- Meet people, laugh, join a community, and build genuine connections with people you are comfortable around.
- Get physically active. You can try light exercises like taking walks, yoga and jogging.
- Choose healthy dietary habits and prioritize eating a balanced diet rich in lean proteins, healthy fats, complex carbohydrates, vitamins, and minerals. Lower your intake of simple sugar and ultra-processed foods (important as insulin spikes and blood glucose fluctuations are also linked to mania19).
- Consider avoiding or limiting caffeine intake, as evidence suggests20 it may impact your condition in unfavorable ways, such as affecting your sleep patterns and interacting with your medication.
- Avoid certain things that can trigger manic episodes21, including listening to loud music, having altercations with loved ones, and starting heavily demanding or creative projects.
- Avoid excessive alcohol consumption and drug misuse.
- You may want to keep a daily journal to note down your symptoms, mood changes, feelings, and observed patterns. This may help you to spot a manic episode early and may also be useful to your healthcare team.
Wrap Up: Awareness Leads to Safety and Support
The onset of a manic episode looks like a pleasant and liberating experience for many. The surge of energy can make you feel powerful, invincible, and special. However, this can be harmful because you are prone to taking high-risk actions and erratic decisions, and can also escalate to depressive symptoms.
It’s important to learn the early signs of mania and also look out for patterns and possible things that trigger an episode for you. This can help ensure safety and early intervention. And getting treatment and care early can help lower the chance of episodes becoming more severe over time.
Learn to be compassionate with yourself and be open to seeking care and accepting support from family and loved ones. While it may seem daunting to live with bipolar disorder, stability and management of symptoms are achievable.