Reading Navigation
Silent Panic Attacks: What They Are & How to Manage Them

The Panic You Can’t See
When you think of the term panic attack you might imagine something noisy, sweaty, lots of visible distress, maybe even heavy breathing into a paper bag, a bottle of water and a collapse in the corner thrown in for good measure. The media likely has some responsibility for this as that’s often how panic is typically portrayed. But the reality for many people is that a panic attack can actually be harder to spot, without a paper bag in sight and without crying. Most importantly sometimes even with the person themselves and those around them having no idea what is actually going on.
What Are Silent Panic Attacks?
Panic symptoms have been described by Dr Elena Borg as “The Silent Cries of The Soul”, a phrase which paints a thousand pictures. It’s the high distress combined with low visibility, silent panic attacks that feel like the duck swimming on a pond looking serene but with legs in overdrive out of sight.
In a nutshell, the physiological symptoms of silent panic are much the same as traditional panic:
- Racing Heart
- Sweating
- Dizziness
- Shortness of Breath
- Chest Pain
- Nausea / Stomach Issues
- Detachment but with a more internal presentation
Learning can be better with an example, so to get a sense of how this presents, here’s a little case study:
“Bernice is a 34-year-old personal trainer and yoga instructor. She was formerly a nurse. She’s a single parent of 2 children. She has started delivering group Yoga classes and is getting consistently positive feedback from her participants. But as soon as she wakes on the day of the session, she feels uneasy. She has an upset stomach and has to go to the bathroom multiple times that day. When greeting her group, she feels an out of body type sensation with a tight chest and a racing heart.
While running the session she worries about not being good enough and has a strong urge to leave the room although she knows she is actually safe. She has a fear she’ll somehow be found out as not being good enough. She feels sweaty but she’s not shaking or hyperventilating, she completes the class without anyone noticing anything was wrong. After the class it takes some hours to return to her baseline, and she wonders why something which went so well felt so frightening. She tends to tell herself she overreacted.”
So, we can see that Bernice is experiencing an activation of her sympathetic nervous system1, which governs the trauma responses like fight, flight, freeze, fawn or flop when we detect a threat. But of course, the invisible nature of her distress makes her think this is ‘just’ anxiety and that there’s something wrong with her for feeling this way.
Discover Support To Match Your Needs
Signs and Symptoms of Silent or Internal Panic Attacks
| Symptom Type | Description |
| Physical/Internal Sensations | Racing heart, dizziness, shortness of breath, tingling, chest tightness, nausea. |
| Cognitive/Emotional Symptoms: | Feeling detached (derealization), fear of losing control, sudden sense of doom. |
| Behavioral Indicators | Freezing, zoning out, avoidance, or subtle escape behaviors. |
Causes and Risk Factors
There are certain factors which can make someone more vulnerable to experiencing silent panic attacks, these include:
Causes:
- Genetics and family history of anxiety or panic disorder
- Chronic stress or unresolved trauma
- Neurobiological sensitivity (fight-or-flight dysregulation)
- Substance use or medication effects
Risk factors:
- Perfectionism
- High-functioning anxiety,
- Major life changes
- Real-world threat triggers such as crowds, driving, caffeine, emotional confrontation
Let’s check back in with Bernice to see what’s around for her:
“Bernice’s mother was raised with alcoholism and depression in her family and as an adult has always struggled with anxiety. Bernice is self-employed with her 2 children to provide for. She often feels her body is quick to tune into things and it will respond even before she’s started having any anxious thoughts. She doesn’t take any medication but does drink one or two cups of coffee a day to help her to focus.”
The Hidden Impact of Panic on Daily Life
Of course, when regularly experiencing panic symptoms2, it can have a big impact on a person’s quality of life. Before too long performance at work can dip, relationships can be affected and self-esteem can take a nosedive. Ultimately, when left unchecked this constant worry can lead to avoidance and also make it more likely that someone will experience symptoms of burnout3. Most importantly the internal conflict and self-blame can often feel all-consuming, and all of this keeps the panic cycle activated.
How to Recognize a Silent Panic Attack (for Yourself and Others)
When in clinic sessions with clients one of the most powerful things I do is to guide them through the “window of tolerance”, a concept developed by Dr. Dan Siegal and Ogden and colleagues4. I’ll share it here and discuss why it matters.
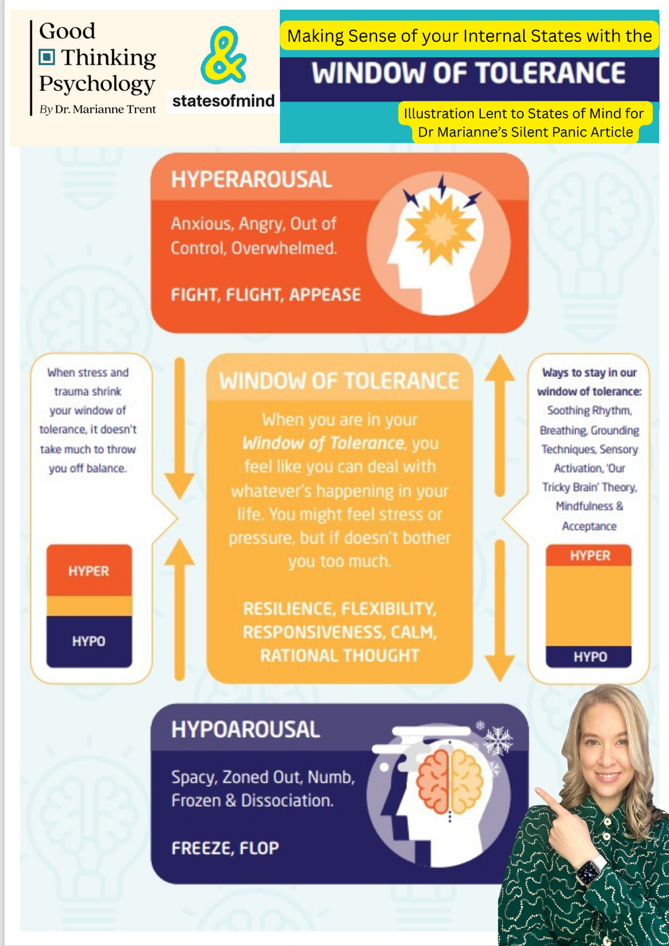
As you can see. It’s a bit like a sandwich. We have Hyperarousal at the top, Hypoarousal at the bottom and in the middle, we are living our lives. When life is going well, we have lots of filling in the middle with thin layers of bread. When we are struggling with trauma, grief, depression or anxiety it can feel like we are all bread and no filling!
Take a look at the features of both Hyperarousal and Hypoarousal. Note the colours associated with each. Learning to pair the experience with the colour can be transformational for people in learning about themselves and treating themselves compassionately as they can understand that these feelings are all indicators of the sympathetic nervous system5 being activated.
So, when we experience feeling anxious, angry, out of control and overwhelmed, we are in the red section. This can often mean we are experiencing heightened arousal which readies our body to ‘fight, flight or fawn/appease’ in the face of stress triggers.
Conversely, when we are in the blue zone, we are likely to experience freeze or flop symptoms, which can include feeling spacy, zoned out, numb, frozen or dissociated. I commonly notice that people might start yawning when they are otherwise well rested. This can be an early warning indicator that they’re starting to edge into the blue section. Understanding this can feel like a powerful road map to your own internal states and therefore give you control to be able to take action.
Let’s check in with Bernice:
Bernice is shallow breathing just in the top section of her throat. She has an intense fear and feels a bit unreal and disconnected from those around her. She feels responsible for the people in her class and when she reviews the window of tolerance in the clinic she notices she is spending lots of time in the red and feels she is putting on an appeasing mask to be able to care for others whilst she is actually experiencing a lot of distress herself. She realises she learned this strategy growing up looking out for her mother and managing conflict between her sisters.
Checklist: Could this be a panic attack?
Body sensations
- Sudden tightness in the chest or throat
- Racing, pounding, or very noticeable heartbeat
- Shortness of breath or feeling you can’t get a full breath
- Dizziness, light-headedness, or feeling “floaty”
- Sweating, flushing, or feeling overheated or cold
- Nausea, upset stomach, or needing the toilet
- Shaking, trembling, or feeling internally “wired”
Mind & thoughts
- A sudden sense of fear or unease that feels out of proportion
- Thoughts like “Something’s wrong”, “I can’t cope”, or “What if I lose control?”
- Difficulty concentrating or thinking clearly
- Feeling detached, unreal, or “not quite here”
Urges & behaviour
- A strong urge to escape, leave, or get to safety
- Wanting reassurance or to check your body repeatedly
- Pushing yourself to stay outwardly calm while feeling overwhelmed inside
Patterns that might fit
- Symptoms peak quickly and then ease (even if it feels long in the moment)
- Medical tests have been reassuring but the symptoms still feel scary
- This tends to happen in situations involving pressure, responsibility, or visibility
- You’re told you “don’t look anxious” but it feels intense internally
Immediate Coping Strategies: What to Do During a Silent Panic Attack
The game changer for what to do is to be able to hold the window of tolerance in mind. Are you in the red or the blue? Notice what physical sensations you’re feeling. Drop your shoulders – I always tell my clients “Let’s just make sure we’re not wearing our shoulders as earrings!”
Then, take a breath. Let me guide you through what we call soothing rhythm breathing.
Soothing Rhythm Breathing
- Take a breath in through your nose. Breathe right down to the bottom of your lungs.
- Notice your diaphragm move as you do. Hold that in breath for a moment.
- Exhale slowly through your mouth. Hold your exhale for a moment.
- This is one cycle. Repeat twice more.
I refer to this as a reset. Even though it may only take a minute it can be transformational and gives you a chance to re-engage your calm, rational brain.
You can also use a 5,4,3,2,1 grounding technique.
- 5 things you can see which show safety (no danger for the bunny here)
- 4 things you can touch or feel (no vibrations through your bunny feet)
- 3 things you can hear (no howling foxes for our bunny)
- 2 things you can smell (no burning or foxes around for the bunny)
- 1 thing you can taste (no poison in the water)
It can also be helpful to develop a mental image of a safe place you can touch base with when you need to borrow a moment of calm. For me I think back to a spa I last went to about 15 years ago. I think of how calm I felt in the sauna. I can feel the warmth and can hear the rainforest sounds being played. I can see the wood panels and the lovely green colours on the forest glazing. I can smell the fragrance. I can remember how it felt to breathe slowly and rhythmically as I enjoyed spending time there. It’s important to note this isn’t dissociation. When connecting with our calm or safe place we are still present in the moment, we are just borrowing a moment of calm to help us to get through tricky moments in the present.
I often find it helpful to address myself gently and compassionately by name. I also remind myself this isn’t my fault and that I’m not the only one to feel this way.
For Bernice this looks like this:
“Come on Bernice. It’s okay. Let’s do this. It’s understandable you feel this way because you’re human and you really care about your class having a good experience.”
Long-Term Management and Prevention — Silent Panic Attack Treatment
If you feel that working through the way you feel with someone after reading this article would be helpful, then I would recommend talking therapies with a qualified and experienced clinician.
The types of therapeutic approaches that can be helpful in understanding and decreasing symptoms of silent panic include:
Compassion Focused Therapy (CFT)
CFT helps you understand yourself as a human and develops a narrative about why you specifically as an individual struggle in the way you. You also develop your own tool kit for how to keep panic at bay for longer and ultimately to take control of it.
Eye Movement Desensitisation & Reprocessing (EMDR)
EMDR6 is often described as a therapy that reaches the parts of the brain that talk-based approaches don’t always access. Trauma can become stored in the nervous system in a way that keeps the body reacting long after the danger has passed. EMDR helps the brain reprocess these memories so they lose their emotional charge and become integrated rather than triggering.
Cognitive Behavioural Therapy (CBT)
If silent panic is a new thing for you without underlying complex trauma history, you could find CBT7 helpful. This can help you think about how your thoughts, feelings, behaviours and bodily sensations are all linked and helps you to break the cycle. This might also include graded exposure to locations or events that make you feel anxious to help you to re-engage with aspects of life you might currently be avoiding.
Mindfulness
Our ‘bunny in the woods’ technique is borrowed from mindfulness so if you found that helpful you may find learning more mindfulness approaches8 is really powerful in helping you take control of the silent panic.
Medication
Medication prescribed by your GP or mental health professional might help you to be able to engage fully with any talking therapy or can help in isolation too.
Lifestyle
Trying to improve your sleep can pay rich dividends for your relationship with anxiety and panic. Similarly, trying to reduce or stop drinking alcohol or unprescribed / recreational drugs can vastly improve the way you feel and reduce the chance of ‘hangxiety’. Caffeine can also fuel anxiety and if you’re regularly experiencing panic and anxiety symptoms trying to reduce or remove caffeine from your diet can be transformational. It’s also worth noting that decaffeinated products such as decaf tea or coffee do still contain caffeine. Only products that are caffeine-free contain no caffeine.
Community, Connection & Empowerment
Panic likes to breed in shame and isolation. Starting to talk about the way you feel can ventilate it enough that it starts to kick it to touch too. Consider connecting with friends or even making new ones. Engaging in hobbies which create a feeling of joy within you can activate your sense of drive and help you feel a sense of mastery.
Ultimately whatever you do, well done for doing it! Consistent changes often have the strongest long-term results.
How to Support Someone Experiencing a Silent Panic Attack
If you are with someone who you think might be experiencing a silent panic attack here are some things which can help.
- Stay calm, speak gently, avoid demanding explanations.
- Phrases that help: “You’re safe,” “I’m here,” “You don’t have to talk right now.”
- What not to say: “Calm down,” “You’re fine,” “It’s all in your head.”
- Check in with them about how they’re feeling once they’ve returned to their normal calmer state.
- If it is affecting their wellbeing, functioning or risk levels encourage them to speak to their GP or mental health professional.
When to Seek Professional Help
There can be some warning signs that things are worsening and would benefit from professional help. These include:
- Frequent or worsening attacks
- Interference with work, relationships, or sleep
- Fear of having another episode which impacts on activities of daily living such as work, leisure, parenting, relationships.
Please, take it from me that reaching out for support doesn’t mean you’re weak. It takes great courage and is your first step towards healing and embracing the life you deserve to be living.
Silent Panic Attacks: You’re Not Alone And You Can Recover
Silent panic attacks are real and a valid reason for why you’re struggling but they are also, ultimately understandable, and treatable too. You’re not broken. You’re not weak. Your nervous system is trying its best to protect you but is just kicking in a bit soon. Silent panic attacks can be dangerous if they impact on your desire to carry on living or interfere with important functions such as driving or crossing the road. You’re not the first or only person to feel this way and being able to access treatment which helps you regain control and live a rich and enjoyable life is key.